Sensitivity Analysis for Likelihood Ratio Models: A Comprehensive Guide for Robust Inference in Biomedical Research
This article provides a comprehensive framework for applying sensitivity analysis to likelihood ratio models in biomedical and clinical research.
Sensitivity Analysis for Likelihood Ratio Models: A Comprehensive Guide for Robust Inference in Biomedical Research
Abstract
This article provides a comprehensive framework for applying sensitivity analysis to likelihood ratio models in biomedical and clinical research. Aimed at researchers, scientists, and drug development professionals, it bridges foundational statistical theory with practical application. The content explores the critical role of sensitivity analysis in quantifying the robustness of model-based inferences to violations of key assumptions, such as unmeasured confounding and missing data mechanisms. It covers methodological implementations, including novel approaches for drug safety signal detection and handling time-to-event data, alongside troubleshooting strategies for common pitfalls like model misspecification and outliers. Finally, the guide presents rigorous validation techniques and comparative analyses to ensure findings are reliable and generalizable, empowering professionals to strengthen the credibility of their statistical conclusions in observational and clinical trial settings.
Core Principles: Understanding Likelihood Ratios and the Imperative for Sensitivity Analysis
Understanding the Core Concept: Likelihood Ratio FAQs
What is a Likelihood Ratio (LR)?
A Likelihood Ratio (LR) is the probability of a specific test result occurring in a patient with the target disorder compared to the probability of that same result occurring in a patient without the target disorder [1]. In simpler terms, it tells you how much more likely a particular test result is in people who have the condition versus those who don't.
How are LRs calculated?
LRs are derived from the sensitivity and specificity of a diagnostic test [2] [1]:
- Positive Likelihood Ratio (LR+) = Sensitivity / (1 - Specificity)
- Negative Likelihood Ratio (LR-) = (1 - Sensitivity) / Specificity
Why are LRs more useful than sensitivity and specificity alone?
Unlike predictive values, LRs are not impacted by disease prevalence [2] [1]. This makes them particularly valuable for:
- Applying test characteristics across different patient populations
- Combining results from multiple diagnostic tests
- Calculating precise post-test probabilities for target disorders
How do I interpret LR values?
The power of an LR lies in its ability to transform your pre-test suspicion into a post-test probability [1]:
| LR Value | Interpretation | Effect on Post-Test Probability |
|---|---|---|
| > 10 | Large increase | Very useful for "ruling in" disease |
| 5-10 | Moderate increase | |
| 2-5 | Small increase | |
| 0.5-2 | Minimal change | Test rarely useful |
| 0.2-0.5 | Small decrease | |
| 0.1-0.2 | Moderate decrease | |
| < 0.1 | Large decrease | Very useful for "ruling out" disease |
Experimental Protocols & Methodologies
Diagnostic Test Validation Protocol
Objective: To determine the sensitivity, specificity, and likelihood ratios of a new diagnostic assay for clinical use.
Materials & Methods:
Patient Cohort Selection: Recruit a representative sample of the target population, ensuring spectrum of disease severity is included.
Reference Standard Application: All participants undergo the "gold standard" diagnostic test to establish true disease status.
Index Test Administration: The new diagnostic test is administered blinded to reference standard results.
Data Collection: Results are recorded in a 2x2 contingency table:
| Disease Present | Disease Absent | |
|---|---|---|
| Test Positive | True Positive (a) | False Positive (b) |
| Test Negative | False Negative (c) | True Negative (d) |
- Statistical Analysis:
- Sensitivity = a/(a+c)
- Specificity = d/(b+d)
- LR+ = Sensitivity/(1-Specificity)
- LR- = (1-Sensitivity)/Specificity
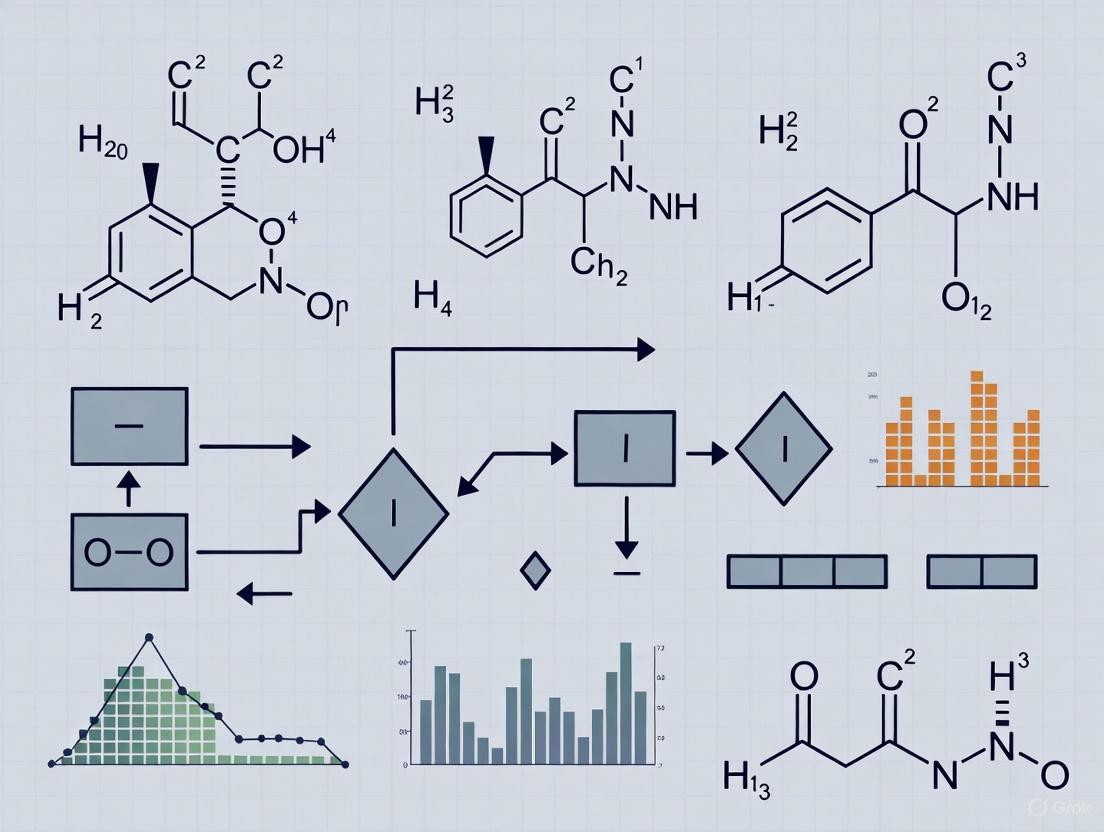
Workflow Visualization:
Application Example: Serum Ferritin for Iron Deficiency
Based on published research [1]:
- Sensitivity: 90% (731/809)
- Specificity: 85% (1500/1770)
- LR+: 6 (90/15)
- LR-: 0.12 (10/85)
Probability Calculation Workflow:
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Resource | Function | Application Context |
|---|---|---|
| Statistical Software (R, Python, SAS) | Calculate LRs, confidence intervals, and precision estimates | Data analysis from diagnostic studies |
| Reference Standard Materials | Establish true disease status for validation studies | Gold standard comparator development |
| Sample Size Calculators | Determine adequate participant numbers for target precision | Study design and power calculations |
| Color Contrast Tools | Ensure accessibility of data visualizations | Creating compliant charts and graphs [3] [4] |
| Material Design Color Palette | Pre-designed accessible color schemes | Data visualization and UI design [5] [6] |
Troubleshooting Common Issues
Problem: Inconsistent LR values across studies
Solution: Consider spectrum bias. Ensure your validation population matches the intended use population. LRs can vary with disease severity and patient characteristics.
Problem: Difficulty communicating LR results to clinicians
Solution: Use visual aids like probability nomograms and consider alternative presentation formats. Research indicates that the optimal way to present LRs to maximize understandability is still undetermined and may require testing different formats with your audience [7].
Problem: Low precision in LR estimates
Solution: Increase sample size. Use confidence intervals to communicate uncertainty. Consider bootstrap methods for interval estimation.
Problem: Integrating multiple test results
Solution: Multiply sequential LRs. If Test A has LR+ = 4 and Test B has LR+ = 5, the combined LR+ = 4 × 5 = 20.
Advanced Applications: Complex Model Comparison
In sensitivity analysis and model comparison, LRs extend beyond diagnostic testing:
Model Selection Protocol:
- Fit competing models to the same dataset
- Calculate likelihoods for each model
- Compute LR = Likelihood(Model A)/Likelihood(Model B)
- Apply decision thresholds based on LR values
- Interpret using similar guidelines as diagnostic LRs
Visualization of Model Comparison:
FAQs: Core Concepts and Common Problems
Q1: What is the fundamental purpose of a sensitivity analysis in statistical inference?
A sensitivity analysis is a method to determine the robustness of an assessment by examining the extent to which results are affected by changes in methods, models, values of unmeasured variables, or assumptions. It addresses "what-if-the-key-inputs-or-assumptions-changed"-type questions, helping to identify which results are most dependent on questionable or unsupported assumptions. When findings are consistent after these tests, the conclusions are considered "robust" [8].
Q2: In the context of likelihood ratio models, my results are sensitive to model specification. How can I troubleshoot this?
This is a common issue when modeling complex relationships. A primary step is to assess the impact of alternative statistical models.
- Action: Conduct a sensitivity analysis by changing the analysis models or modifying the functional form. For instance, if using a linear model, consider if a generalized linear model is more appropriate. Compare the results from these different models against your primary analysis.
- Goal: Identify if your key conclusions (e.g., statistical significance of a treatment effect) change under different plausible modeling approaches. A lack of change strengthens the credibility of your findings [9] [8].
Q3: My likelihood ratio test for a meta-analysis has low power. What are potential causes and solutions?
Low power in this context can stem from the model's complexity and the estimation method used.
- Cause: The increased complexity of models like location-scale meta-analysis models can make fitting challenging and impact the performance of statistical tests.
- Solution: A simulation study found that using Restricted Maximum Likelihood (REML) estimation can yield better statistical properties, such as Type I error rates closer to the nominal level. Furthermore, the Likelihood-Ratio Test (LRT) itself was shown to achieve the highest statistical power compared to Wald-type or permutation tests, making it a good choice for detecting true effects [10].
Q4: How do I quantify the robustness of a causal inference from an observational study?
For causal claims, specialized sensitivity analysis techniques are required to quantify how strong an unmeasured confounder would need to be to alter the inference.
- Technique 1: Robustness of Inference to Replacement (RIR): This method answers: "To invalidate the inference, what percentage of the data would have to be replaced with counterfactual cases for which the treatment had no effect?" [11]
- Technique 2: Impact Threshold for a Confounding Variable (ITCV): This technique answers: "An omitted variable would have to be correlated at _ with the predictor of interest and with the outcome to change the inference." [11]
- Tool: These analyses can be conducted in R using the
pkonfoundcommand or via the online appkonfound-it[11].
Troubleshooting Guides
Guide 1: Handling Protocol Deviations and Non-Compliance in Clinical Trials
Problem: Participants in a randomized controlled trial (RCT) do not adhere to the prescribed intervention, potentially diluting the observed treatment effect and biasing the results.
Solution Steps:
- Primary Analysis: First, perform an Intention-to-Treat (ITT) analysis, where participants are analyzed according to the group to which they were originally randomized, regardless of what treatment they actually received. This is the standard primary analysis for RCTs.
- Sensitivity Analyses: Perform the following sensitivity analyses to test the robustness of your ITT conclusion:
- Per-Protocol (PP) Analysis: Exclude participants who majorly violated the study protocol from the analysis. This estimates the effect under ideal conditions.
- As-Treated (AT) Analysis: Analyze participants based on the treatment they actually received, rather than the one they were assigned to.
- Interpretation: Compare the results of the ITT, PP, and AT analyses. If all three lead to the same qualitative conclusion (e.g., the intervention is effective), your result is considered robust. If they differ, you must discuss the potential reasons and implications in your report [8].
Guide 2: Assessing Robustness to Unmeasured Confounding
Problem: In an observational study assessing a new drug's effect, a critic argues that your finding could be explained by an unmeasured variable (e.g., socioeconomic status).
Solution Steps:
- Calculate the E-value: The E-value quantifies the minimum strength of association that an unmeasured confounder would need to have with both the treatment and the outcome to fully explain away the observed effect. It can be calculated for both the effect estimate and the confidence interval limits.
- Benchmarking: Compare the E-value to the strengths of association of measured confounders in your model. If the E-value is much larger than the associations you have already accounted for, it suggests that an unmeasured confounder would need to be unrealistically strong to negate your result.
- Reporting: Clearly report the E-value alongside your main results. For example: "The hazard ratio for the drug's effect was 0.62 (95% CI: 0.48, 0.79). The E-value was 2.84, indicating that an unmeasured confounder would need to be associated with both treatment and outcome by risk ratios of 2.84-fold each to explain away the effect, which is stronger than any measured confounder in our study" [9].
Key Experimental Protocols
Protocol 1: Simulation Study for Evaluating a New Likelihood Ratio Test
This protocol is adapted from studies that evaluate statistical tests through Monte Carlo simulation [10] [12].
Objective: To compare the performance (Type I error rate and statistical power) of a proposed Empirical Likelihood Ratio Test (ELRT) against a standard test (e.g., Ljung-Box test) for identifying an AR(1) time series model.
Methodology:
- Data Generation: Generate multiple (e.g., 10,000) synthetic time series datasets under two scenarios:
- Null Hypothesis (H₀): Data are generated from a true AR(1) model to assess Type I error rate.
- Alternative Hypothesis (H₁): Data are generated from a different model (e.g., AR(2)) to assess statistical power.
- Model Application: On each generated dataset, apply both the proposed ELRT and the standard Ljung-Box test.
- Performance Calculation:
- Empirical Type I Error: Calculate the proportion of times the tests incorrectly reject H₀ when H₀ is true. This should be close to the chosen significance level (e.g., 5%).
- Empirical Power: Calculate the proportion of times the tests correctly reject H₀ when H₁ is true.
Expected Workflow:
Protocol 2: Sensitivity Analysis for Observational Study on Drug Effects
This protocol is based on reviews of best practices in studies using routinely collected healthcare data [9].
Objective: To assess the robustness of a primary analysis estimating a drug's treatment effect against potential biases from study definitions and unmeasured confounding.
Methodology:
- Primary Analysis: Conduct the pre-specified main analysis (e.g., a multivariable Cox regression) on the primary outcome.
- Sensitivity Analyses: Plan and execute a series of sensitivity analyses. The table below summarizes the types and examples.
- Comparison and Interpretation: Systematically compare the effect estimates from all sensitivity analyses with the primary analysis. Quantify the difference (e.g., a 24% average difference in effect size was observed in some studies [9]) and discuss the implications of any inconsistencies.
Sensitivity Analysis Framework:
Data Presentation
Table 1: Common Types of Sensitivity Analyses and Their Applications
| Analysis Type | Description | When to Use | Example from Literature |
|---|---|---|---|
| Alternative Study Definitions | Using different algorithms or codes to define exposure, outcome, or confounders. | When classifications based on real-world data (e.g., ICD codes) might be misclassified. | In a drug study, varying the grace period for defining treatment discontinuation [9]. |
| Alternative Study Designs | Using a different data source or changing the inclusion criteria for the study population. | To test if findings are specific to a particular population or data collection method. | Comparing results from a primary data analysis to those from a validation cohort [9]. |
| Alternative Modeling | Changing the statistical model, handling of missing data, or testing assumptions. | When model assumptions (e.g., linearity, normality) are in question or to address missing data. | Using multiple imputation instead of complete-case analysis for missing data [9] [8]. |
| Impact of Outliers | Re-running the analysis with and without extreme values. | When the data contain values that are numerically distant from the rest and may unduly influence results. | A cost-effectiveness analysis where excluding outliers changed the cost per QALY ratio [8]. |
| Protocol Deviations | Performing Per-Protocol or As-Treated analyses alongside the primary ITT analysis. | Essential for RCTs where non-compliance or treatment switching is present. | A trial where ITT showed no effect, but a sensitivity analysis on compliers found a significant effect [8]. |
Table 2: Comparison of Tests in a Simulation Study for AR(1) Model Identification
| Test Method | Empirical Size (α=0.05) | Statistical Power | Key Findings |
|---|---|---|---|
| Empirical Likelihood Ratio Test (ELRT) | Maintains nominal size accurately | Superior power | More reliable for identifying the correct AR(1) model structure compared to the Ljung-Box test [12]. |
| Ljung-Box (LB) Test | Less accurate empirical size | Lower power | As an omnibus test, it can be less powerful for specifically detecting departures from an AR(1) model [12]. |
The Scientist's Toolkit: Research Reagent Solutions
Software and Packages
- R and
pkonfound: For conducting sensitivity analyses for causal inference using RIR and ITCV methods [11]. - R and
metafor: A key package for fitting location-scale meta-analysis models and performing likelihood ratio tests, supporting both ML and REML estimation [10]. konfound-itWeb App: A user-friendly, code-free interface for running sensitivity analyses for causal inferences. Accessible at http://konfound-it.com [11].
Methodological Frameworks
- Robustness of Inference to Replacement (RIR): A framework to quantify how many cases would need to be replaced with non-responsive cases to change a statistical inference [11].
- Impact Threshold for a Confounding Variable (ITCV): A framework to quantify how strong an unmeasured confounder would need to be to change an inference [11].
- E-value: A single number that summarizes the minimum strength of association an unmeasured confounder would need to have to explain away a treatment-outcome association [9].
Troubleshooting Guides
Guide 1: Addressing Unmeasured Confounding in Observational Studies
Problem: A researcher is concerned that an observed causal effect between a new drug and patient recovery might be biased due to an unmeasured confounder, such as socioeconomic status.
Diagnosis: The E-value is a quantitative measure that can assess how strong an unmeasured confounder would need to be to explain away the observed treatment effect [13]. A small E-value suggests your results are robust to plausible confounding, while a large E-value indicates fragility.
Solution:
- Calculate the E-value for your point estimate and confidence intervals [13].
- Interpret the E-value in the context of your field's knowledge. Could a confounder of this strength reasonably exist?
- Report the E-value alongside your causal effect estimate to transparently communicate robustness.
Guide 2: Handling Noncompliance in Randomized Controlled Trials (RCTs)
Problem: In an RCT, participant noncompliance to the assigned treatment protocol means the treatment received is not randomized, potentially biasing the causal effect of the treatment actually received [14].
Diagnosis: Standard Intention-to-Treat (ITT) analysis gives the effect of treatment assignment, not the causal effect of the treatment itself. When compliance is imperfect, other methods are needed.
Solution: Several estimators can be used when compliance is measured with error [14]:
- Inverse Probability of Compliance Weighted (IPCW) Estimators: Model the probability of compliance given confounders to create a weighted pseudo-population where treatment is independent of confounders [14].
- Regression-Based Estimators: Model the conditional mean of the response given confounders, treatment, and (estimated) compliance status [14].
- Doubly-Robust Augmented Estimators: Combine the IPCW and regression approaches. This estimator is consistent if either the regression model or the model for the probability of compliance is correctly specified, making it more robust to model misspecification [14].
Guide 3: Managing Non-Ignorable Loss to Follow-Up
Problem: Outcome data are missing because participants drop out of a study (Loss to Follow-Up), and the missingness is related to the unobserved outcome itself. This is known as Missing Not at Random (MNAR) data, which can severely bias causal effect estimates [15].
Diagnosis: Standard imputation methods assume data are Missing at Random (MAR). When this assumption is violated, sensitivity analysis is required.
Solution: Implement a multiple-imputation-based pattern-mixture model [15]:
- Define one or more plausible MNAR mechanisms (e.g., participants with worse outcomes are more likely to drop out).
- Impute the missing data multiple times under each specified MNAR mechanism.
- Analyze the completed datasets and pool the results.
- Compare the causal effect estimates across the different MNAR scenarios to test the robustness of your original conclusion [15].
Frequently Asked Questions (FAQs)
Q1: What does a "robust" finding actually mean in causal inference? A robust finding is one that does not change substantially when key assumptions are tested or violated. This includes being insensitive to plausible unmeasured confounding, different model specifications, or non-ignorable missing data mechanisms [13] [14] [15]. Robustness does not prove causality, but it significantly increases confidence in the causal conclusion.
Q2: My analysis found a significant effect, but the E-value is low. What should I do? A low E-value indicates that a relatively weak unmeasured confounder could negate your observed effect. You should [13]:
- Acknowledge this limitation transparently in your reporting.
- Use prior knowledge to argue whether a confounder of such strength is likely.
- Consider designing a follow-up study that directly measures and adjusts for the suspected confounder.
Q3: What is the practical difference between "doubly-robust" estimators and other methods? Doubly-robust estimators provide two chances for a correct inference. They will yield a consistent causal estimate if either your model for the treatment (or compliance) mechanism or your model for the outcome is correctly specified [14]. This is a significant advantage over methods that require a single model to be perfectly specified, which is often an unrealistic assumption in practice.
Q4: How do I choose which sensitivity analysis to use? The choice depends on your primary threat to validity:
- For unmeasured confounding in observational studies, use the E-value or Rosenbaum bounds [13].
- For noncompliance in RCTs, use IPCW, regression, or doubly-robust estimators [14].
- For non-ignorable missing outcome data, use pattern-mixture models or other MNAR sensitivity analyses [15].
Quantitative Data Tables
Table 1: Comparison of Sensitivity Analysis Methods for Causal Inference
| Method | Primary Use Case | Key Inputs | Interpretation of Result | Key Assumptions |
|---|---|---|---|---|
| E-value [13] | Unmeasured confounding | Risk Ratio, Odds Ratio | Strength of confounder needed to explain away the effect | Confounder must be associated with both treatment and outcome. |
| Rosenbaum Bounds [13] | Unmeasured confounding in matched studies | Sensitivity parameter (Γ) | Range of p-values or effect sizes under varying confounding | Specifies the degree of hidden bias. |
| Doubly-Robust Estimators [14] | Noncompliance, general model misspecification | Treatment and outcome models | Causal effect estimate | Consistent if either the treatment or outcome model is correct. |
| Tipping Point Analysis [13] | Unmeasured confounding | Effect estimate, confounder parameters | The confounder strength that changes study conclusions | Pre-specified assumptions about confounder prevalence. |
Table 2: Scenario Analysis for Non-Ignorable Loss to Follow-Up
| MNAR Scenario | Imputation Model Adjustment | Impact on Causal Risk Ratio (Example) | Robustness Conclusion |
|---|---|---|---|
| Base Case (MAR) | None | 0.75 (0.60, 0.95) | Reference |
| Scenario 1: Mild MNAR | Dropouts 20% more likely to have event | 0.78 (0.62, 0.98) | Robust (Conclusion unchanged) |
| Scenario 2: Severe MNAR | Dropouts 50% more likely to have event | 0.85 (0.68, 1.06) | Not Robust (CI includes null) |
| Scenario 3: Protective MNAR | Dropouts 20% less likely to have event | 0.73 (0.58, 0.92) | Robust (Conclusion unchanged) |
Experimental Protocols
Protocol 1: Implementing a Sensitivity Analysis for Unmeasured Confounding using the E-value
Objective: To quantify the robustness of a causal risk ratio (RR) to potential unmeasured confounding.
Materials: Your dataset, statistical software (e.g., R, Stata).
Procedure:
- Estimate the Causal Effect: Fit your primary model to obtain the adjusted Risk Ratio (RR) and its confidence interval (CI).
- Calculate the E-value: Compute the E-value for the point estimate and the CI limit closest to the null.
- The E-value for an RR is calculated as:
E-value = RR + sqrt(RR * (RR - 1))for RR > 1. For RR < 1, first take the inverse of the RR (1/RR).
- The E-value for an RR is calculated as:
- Interpret the Result: The E-value represents the minimum strength of association that an unmeasured confounder would need to have with both the treatment and the outcome, on the risk ratio scale, to fully explain away the observed association [13].
- Report: Present the E-values alongside your primary result to communicate its sensitivity.
Protocol 2: Applying a Doubly-Robust Estimator for Noncompliance in an RCT
Objective: To estimate the causal effect of treatment received in the presence of noncompliance, with robustness to model misspecification.
Materials: RCT data including: randomized treatment assignment (A), treatment actually received (Z), outcome (Y), and baseline covariates (X).
Procedure:
- Specify Models:
- Treatment/Compliance Model: A model (e.g., logistic regression) for the probability of receiving treatment given randomization and covariates,
P(Z|A, X). - Outcome Model: A model (e.g., linear regression) for the expected outcome given randomization, treatment received, and covariates,
E(Y|A, Z, X).
- Treatment/Compliance Model: A model (e.g., logistic regression) for the probability of receiving treatment given randomization and covariates,
- Estimate Parameters: Fit both models to the observed data.
- Construct the Estimator: Implement the augmented inverse probability weighted (AIPW) estimator [14]. This involves: a. Calculating inverse probability weights from the treatment model. b. Using the outcome model to predict counterfactual outcomes under full compliance. c. Combining these components into a single, "augmented" estimator.
- Validate: The estimator is consistent if either the treatment model or the outcome model is correctly specified. Check the sensitivity of your result by varying the specifications of both models [14].
Signaling Pathways & Workflows
Diagram 1: Robustness Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table: Key Analytical Tools for Robust Causal Inference
| Tool / Method | Function in Analysis | Key Property / Advantage |
|---|---|---|
| E-value [13] | Quantifies the required strength of an unmeasured confounder. | Intuitive and easy-to-communicate metric for sensitivity. |
| Rosenbaum Bounds [13] | Assesses sensitivity of results in matched observational studies. | Does not require specifying the exact nature of the unmeasured confounder. |
| Doubly-Robust Estimator [14] | Estimates causal effects in the presence of noncompliance or selection bias. | Provides two chances for correct inference via dual model specification. |
| Pattern-Mixture Models [15] | Handles missing data that is Missing Not at Random (MNAR). | Allows for explicit specification of different, plausible missing data mechanisms. |
| Inverse Probability Weighting [14] | Corrects for selection bias or confounding by creating a pseudo-population. | Directly addresses bias from missing data or treatment allocation. |
Frequently Asked Questions
What is the primary goal of a sensitivity analysis? Sensitivity analysis determines the robustness of a study's findings by examining how results are affected by changes in methods, models, values of unmeasured variables, or key assumptions. It addresses "what-if" questions to see if conclusions change under different plausible scenarios [16] [8].
My clinical trial has missing data. What is the first step in handling it? The first step is to assess the missing data mechanism. Is it Missing Completely at Random (MCAR), Missing at Random (MAR), or Missing Not at Random (MNAR)? This classification guides the choice of appropriate analytical methods, as MNAR data, in particular, introduce a high risk of bias and require specialized techniques like sensitivity analysis [17].
A reviewer is concerned about unmeasured confounding in our observational study. How can I address this? Sensitivity analysis for unmeasured confounding involves quantifying how strong an unmeasured confounder would need to be to alter the study's conclusions. This can be done by simulating the influence of a hypothetical confounder or using statistical techniques like the Delta-Adjusted approach within multiple imputation to assess the robustness of your results [17] [18].
We had significant protocol deviations in our RCT. Which analysis should be our primary one? The Intention-to-Treat (ITT) analysis, where participants are analyzed according to the group they were originally randomized to, is typically the primary analysis as it preserves the randomization. Sensitivity analyses, such as Per-Protocol (PP) or As-Treated (AT) analyses, should then be conducted to assess the robustness of the ITT findings to these deviations [16] [8].
How do I choose parameters for a sensitivity analysis? The choice should be justified based on theory, prior evidence, or expert opinion. It is crucial to vary parameters over realistic and meaningful ranges. For multiple parameters, consider their potential correlations and use methods like multivariate sensitivity analysis to account for this interplay [19].
Troubleshooting Guides
Issue 1: Handling Missing Data in Time-to-Event Analyses
- Problem: Loss to follow-up in a longitudinal study leads to missing time-dependent covariates in a Cox proportional hazards model, potentially biasing survival estimates [17].
- Investigation: Check the proportion and patterns of missing data. If more than 5% of data are missing, simple methods like Complete Case Analysis (CCA) are likely inadequate and can produce biased estimates [17].
- Solution: Implement a structured approach to handle different missing data mechanisms.
- Protocol:
- Specify the Mechanism: Pre-specify in your analysis plan whether you assume data are MAR or NMAR.
- Primary Analysis (MAR): Use Multiple Imputation (MI) to handle missing data under the MAR assumption. Incorporate event-related variables (event indicator, event time) into the imputation model to maintain consistency with the Cox model [17].
- Sensitivity Analysis (NMAR): To assess robustness, use the Delta-Adjusted Multiple Imputation method. This modifies the imputed values by introducing a sensitivity parameter (delta, δ) to reflect plausible departures from the MAR assumption.
- Create multiple versions of the imputed dataset with different delta values.
- Re-run your Cox model on each dataset.
- Compare the range of treatment effect estimates (e.g., hazard ratios) across these scenarios [17].
- Interpretation: If the conclusions from your primary MAR analysis remain consistent across various NMAR scenarios explored with delta-adjustments, your results are considered robust to missing data assumptions [17].
Issue 2: Addressing Protocol Deviations in Randomized Controlled Trials
- Problem: Participants do not adhere to the assigned treatment (non-compliance) or violate the study protocol, potentially diluting the measured treatment effect [8].
- Investigation: Classify the types of deviations (e.g., crossovers, non-adherence, incomplete treatment) and determine which participants are affected.
- Solution: Perform complementary analyses to the primary ITT analysis.
- Protocol:
- Primary Analysis: Conduct an Intention-to-Treat (ITT) analysis. Analyze all participants in the groups they were originally randomized to, regardless of what treatment they actually received.
- Sensitivity Analyses:
- Per-Protocol (PP) Analysis: Restrict the analysis only to participants who complied with the protocol without major violations.
- As-Treated (AT) Analysis: Analyze participants according to the treatment they actually received, regardless of randomization.
- Interpretation: The ITT analysis provides a conservative, "real-world" estimate of effectiveness. If the PP and AT analyses yield results that are consistent in direction and significance with the ITT analysis, confidence in the robustness of the treatment effect is greatly increased [16] [8].
Issue 3: Accounting for Unmeasured Confounding
- Problem: An observational study or external comparator analysis finds an association, but a critic argues that an unmeasured variable could explain the result [18].
- Investigation: Identify potential key confounders that were not collected (e.g., socioeconomic status, genetic factors, disease severity) and hypothesize how they might be related to both the treatment and the outcome.
- Solution: Quantify the potential impact of an unmeasured confounder through simulation or probabilistic bias analysis.
- Protocol: One common approach is to simulate a confounding variable:
- Define Parameters: Make assumptions about the prevalence of the unmeasured confounder in the treatment and control groups and its strength of association with the outcome.
- Adjust the Model: Incorporate this simulated confounder into your statistical model (e.g., a Cox regression or logistic regression) as an additional covariate.
- Iterate: Repeat the analysis across a range of plausible values for the confounder's prevalence and strength.
- Alternative Method: For studies using propensity score weighting, you can simulate how the inclusion of a strong unmeasured confounder would affect the propensity scores and, consequently, the balance between groups and the final estimate [18].
- Interpretation: The analysis shows how much the unmeasured confounder would need to influence the treatment and outcome to change the study's conclusion (e.g., to render a significant result non-significant). This provides a quantitative argument for the robustness of your findings [18].
Table 1: Summary of Sensitivity Analysis Methods for Key Scenarios
| Scenario | Primary Method | Sensitivity Analysis Method(s) | Key Quantitative Measures |
|---|---|---|---|
| Missing Data | Multiple Imputation (assuming MAR) [17] | Delta-Adjusted Multiple Imputation (for NMAR) [17] | Delta (δ) shift values; Range of hazard ratios/coefficients across imputations |
| Protocol Deviations | Intention-to-Treat (ITT) Analysis [8] | Per-Protocol Analysis; As-Treated Analysis [8] | Comparison of treatment effect estimates (e.g., odds ratio, mean difference) between ITT and sensitivity analyses |
| Unmeasured Confounding | Standard Multivariable Regression | Simulation of Hypothetical Confounder; Probabilistic Bias Analysis [18] | E-value; Strength and prevalence of confounder required to nullify the observed effect |
Detailed Protocol: Delta-Adjusted Multiple Imputation for Missing Data [17]
- Imputation Model Setup: Use a Multiple Imputation by Chained Equations (MICE) framework. Ensure the imputation model includes the event indicator, event/censoring time, and other relevant covariates to preserve the relationship with the time-to-event outcome.
- Baseline Imputation: Generate
mcomplete datasets (e.g., m=20) under the MAR assumption. - Delta-Adjustment: For scenarios exploring NMAR, select a sensitivity parameter
δ. This parameter represents a systematic shift (e.g., adding a fixed value or a multiple of the standard deviation) to the imputed values for missing observations.- For example, if
Y_obsis the mean of the observed data, imputed valuesY_impcould be set toY_obs + δ.
- For example, if
- Analysis: Fit your primary statistical model (e.g., Cox regression) to each of the
mdelta-adjusted datasets. - Pooling: Combine the results from the
manalyses using Rubin's rules to obtain an overall estimate of the treatment effect and its variance for that specificδvalue. - Sensitivity Exploration: Repeat steps 3-5 for a range of plausible
δvalues (both positive and negative) to create a "sensitivity landscape" for your results.
The Scientist's Toolkit
Table 2: Essential Reagents & Resources for Sensitivity Analysis
| Item | Function in Analysis |
|---|---|
| Statistical Software (R/Stata) | Provides the computational environment and specialized packages (e.g., mice in R, mi in Stata) for implementing multiple imputation and complex modeling [19] [17]. |
| Multiple Imputation Package | Automates the process of creating multiple imputed datasets and pooling results, which is essential for handling missing data under MAR and NMAR assumptions [17]. |
| Sensitivity Parameter (δ) | A user-defined value used in delta-adjustment methods to quantify and test departures from the MAR assumption, allowing researchers to explore NMAR scenarios [17]. |
| Propensity Score Modeling | A technique used in observational studies to adjust for measured confounding by creating a single score that summarizes the probability of receiving treatment given covariates. It forms the basis for weighting (ATE, ATT, ATO) and matching [18]. |
Methodological Workflows
Sensitivity Analysis Decision Workflow
FAQs: Core Concepts and Workflow Design
Q1: What is the fundamental connection between primary analysis and robustness assessment in drug development? A robust primary analysis is the foundation, but it is not sufficient on its own. Robustness assessment, often through sensitivity analysis, is a critical subsequent step that tests how much your primary results change under different, but plausible, assumptions. This is especially important when data may be Missing Not at Random (MNAR), where the fact that data is missing is itself informative. For instance, in a clinical trial, if patients experiencing more severe side effects drop out, their data is MNAR. A primary analysis might assume data is Missing at Random (MAR), but a robustness assessment would test how sensitive the conclusion is to various MNAR scenarios [17].
Q2: How do I structure a workflow to ensure my analytical process is robust? A robust analytical workflow is structured and reproducible. It should include the following key stages [20]:
- Data Acquisition & Extraction: Collect data in standardized formats and create a data dictionary to document each element. Use version control and automate extraction where possible.
- Data Cleaning & Preprocessing: Handle missing values, detect inconsistencies, and encode variables appropriately. Document all steps.
- Modeling & Statistical Analysis: Start with simple models before moving to complex ones. Document all methods, results, and key decisions.
- Validation: Use training, validation, and test datasets. Conduct peer reviews and audits to ensure results are reproducible.
- Reporting & Visualization: Communicate insights clearly with simple visualizations and automated reports to ensure findings are utilized effectively.
Q3: What is a Robust Parameter Design and how is it used? Pioneered by Dr. Genichi Taguchi, Robust Parameter Design (RPD) is an experimental design method used to make a product or process insensitive to "noise factors"—variables that are difficult or expensive to control during normal operation [21] [22]. The goal is to find the optimal settings for the control factors (variables you can control) that minimize the response variation caused by noise factors. For example, a cake manufacturer can control ingredients (control factors) but not a consumer's oven temperature (noise factor). RPD helps find a recipe that produces a good cake across a range of oven temperatures [22].
Q4: What is the Delta-Adjusted Multiple Imputation (DA-MI) approach and when should I use it? DA-MI is a sensitivity analysis technique used when dealing with potentially MNAR data [17]. It starts with a standard Multiple Imputation (which assumes MAR) and then systematically adjusts the imputed values using a sensitivity parameter, delta (δ), to simulate various degrees of departure from the MAR assumption. You should use this method to test the robustness of your results, especially in longitudinal studies where dropouts may be related to the outcome, such as in time-to-event analyses in clinical trials [17].
Troubleshooting Common Experimental Issues
Problem: Inconsistent or non-reproducible results after implementing a Robust Parameter Design.
- Potential Cause: The design may have been improperly fractionated, leading to severe aliasing where the effect of one factor is confused with the effect of another factor or an interaction [22].
- Solution: Verify the design's properties before experimentation. For two-level RPDs, check the generalized resolution and generalized minimum aberration. Designs with higher resolution and lower aberration are preferred as they reduce serious aliasing. Use statistically validated design patterns rather than creating them from scratch without expert knowledge [22].
Problem: Analytical workflow is efficient but results are misleading.
- Potential Cause: Inadequate data cleaning and preprocessing, or "overfitting" where a model is too complex and captures noise instead of the underlying signal [20].
- Solution:
- Reinvest in the data cleaning stage: implement rigorous checks for missing data, inconsistencies, and duplicates.
- For machine learning models, ensure you use a separate training set to build the model, a validation set to tune parameters, and a test set only for the final evaluation to prevent overfitting.
- Benchmark your model's performance against simpler, well-established methods [20].
Problem: Difficulty communicating the uncertainty from a likelihood ratio or sensitivity analysis to non-statistical stakeholders.
- Potential Cause: The format used to present statistical strength (e.g., likelihood ratios) may be difficult for laypersons to comprehend [7].
- Solution: Research indicates that the format of presentation impacts understanding. Move beyond presenting only numerical likelihood ratios. Use a combination of formats:
Experimental Protocols for Robustness Assessment
Protocol 1: Conducting a Sensitivity Analysis using Delta-Adjusted Multiple Imputation
This protocol is for assessing the robustness of a Cox proportional hazards model with missing time-dependent covariate data [17].
1. Primary Analysis (Under MAR):
- Use Multiple Imputation by Chained Equations (MICE) to create
mcomplete datasets (e.g., m=20), assuming the data is Missing at Random. - Fit the Cox model to each of the
mdatasets. - Pool the results using Rubin's rules to get the primary estimate of the treatment effect (e.g., Hazard Ratio).
2. Sensitivity Analysis (Exploring NMAR via Delta-Adjustment):
- Define a set of plausible delta (δ) values. These represent the systematic shift applied to imputed values. For example, δ = { -0.5, -0.2, +0.2, +0.5 }.
- For each value of δ in the set:
- Modify the imputation model used in the MICE procedure by adding the δ value to the imputed values for the missing data.
- Generate a new set of
mimputed datasets under this specific NMAR scenario. - Fit the Cox model to each dataset and pool the results.
- Compare the range of treatment effects (e.g., Hazard Ratios) and their confidence intervals across all δ scenarios to the primary MAR estimate.
3. Interpretation:
- If the conclusion about the treatment effect (e.g., statistical significance or direction of effect) does not change across the range of plausible δ values, the result is considered robust to departures from the MAR assumption.
- If the conclusion changes, this indicates the finding is sensitive to the assumptions about the missing data, and this uncertainty must be reported.
Protocol 2: Executing a Robust Parameter Design Experiment
This protocol outlines the steps to minimize a product's/process's sensitivity to noise factors [21] [22].
1. Problem Formulation with P-Diagram:
- Create a P-Diagram to classify variables.
- Signal (Input): The intended command or setting.
- Response (Output): The desired performance characteristic.
- Control Factors: Parameters you can specify and control.
- Noise Factors: Hard-to-control variables that cause variation.
- Ideal Function: The perfect theoretical relationship between signal and response.
2. Experimental Planning:
- Select an appropriate Orthogonal Array (a highly fractionated factorial design) for the experiment. This array should accommodate your control and noise factors with a minimal number of experimental runs.
- The design is denoted as 2^(m1+m2)-(p1-p2), where m1 is control factors, m2 is noise factors, p1/p2 are fractionation levels [22].
3. Experimentation and Analysis:
- Run the experiment according to the orthogonal array. For each run, expose the system to different combinations of controlled noise factors.
- For each experimental run, calculate the Signal-to-Noise (S/N) Ratio. This metric, derived from Taguchi's Quadratic Loss Function, measures robustness by combining the mean and variance of the response; a higher S/N ratio indicates lower sensitivity to noise [21].
- Use the data to perform two optimization steps:
- Variance Reduction: Identify control factor settings that maximize the S/N ratio.
- Mean Adjustment: Use a "scaling factor" (a control factor that affects the mean but not the S/N ratio) to adjust the mean response to the target value [21].
Workflow and Pathway Visualizations
Analytical Robustness Workflow
P-Diagram for Robust Design
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details key methodological and informational resources for conducting robust analyses in drug development.
| Tool / Resource Name | Type | Function / Purpose |
|---|---|---|
| Robust Parameter Design (Taguchi Method) [21] [22] | Statistical Experimental Design | Systematically finds control factor settings to minimize output variation caused by uncontrollable noise factors. |
| Delta-Adjusted Multiple Imputation (DA-MI) [17] | Sensitivity Analysis Method | Tests the robustness of statistical inferences to deviations from the Missing at Random (MAR) assumption in datasets with missing values. |
| P-Diagram [21] | Conceptual Framework Tool | Classifies variables into signal, response, control, and noise factors to succinctly define the scope of a robustness problem. |
| Orthogonal Arrays [21] [22] | Experimental Design Structure | Allows for the efficient and reliable investigation of a large number of experimental factors with a minimal number of test runs. |
| Signal-to-Noise (S/N) Ratio [21] | Robustness Metric | A single metric used in parameter design to predict field quality and find factor settings that minimize sensitivity to noise. |
| FDA Fit-for-Purpose (FFP) Initiative [23] | Regulatory Resource | Provides a pathway for regulatory evaluation and acceptance of specific drug development tools (DDTs), including novel statistical methods, for use in submissions. |
| Drug Development Tools (DDT) Qualification Programs [24] | Regulatory Resource | FDA programs that guide submitters as they develop tools (e.g., biomarkers, clinical outcome assessments) for a specific Context of Use (COU) in drug development. |
Implementation in Practice: Techniques for Applying Sensitivity Analysis to LR Models
What is the Likelihood Ratio Test and what is its primary purpose?
The Likelihood Ratio Test (LRT) is a statistical hypothesis test used to compare the goodness-of-fit between two competing models. Its primary purpose is to determine if a more complex model (with additional parameters) fits a particular dataset significantly better than a simpler, nested model. The simpler model must be a special case of the more complex one, achievable by constraining one or more of the complex model's parameters [25]. The LRT provides an objective criterion for deciding whether the improvement in fit justifies the added complexity of the additional parameters [25].
How does the LRT work? What is the underlying logic?
The underlying logic of the LRT is to compare the maximum likelihood achievable by each model. The test statistic is calculated as the ratio of the maximum likelihood of the simpler model (the null model) to the maximum likelihood of the more complex model (the alternative model) [26]. For convenience, this ratio is transformed into a log-likelihood ratio statistic [27]:
λ_LR = -2 * ln[ L(null model) / L(alternative model) ] = -2 * [ ℓ(null model) - ℓ(alternative model) ]
where ℓ represents the log-likelihood [26]. A large value for this test statistic indicates that the complex model provides a substantially better fit to the data than the simple model. According to Wilk's Theorem, as the sample size approaches infinity, this test statistic follows a chi-square distribution under the null hypothesis [27]. The degrees of freedom for this chi-square distribution are equal to the difference in the number of free parameters between the two models [25].
A Practical Example: Testing a Molecular Clock
The following table summarizes a hypothetical experiment to test whether a DNA sequence evolves at a constant rate (i.e., follows a molecular clock) [25].
| Model Description | Log-Likelihood (ℓ) | Number of Parameters |
|---|---|---|
| Null (H₀): HKY85 model with a molecular clock (simpler model) | ℓ₀ = -7573.81 | Fewer parameters (rate homogeneous across branches) |
| Alternative (H₁): HKY85 model without a molecular clock (more complex model) | ℓ₁ = -7568.56 | More parameters (rate varies across branches) |
LRT Calculation and Interpretation:
- Calculate the test statistic: λ_LR = -2 * (ℓ₀ - ℓ₁) = -2 * (-7573.81 - (-7568.56)) = 10.50 [25]
- Determine the degrees of freedom: df = s - 2, where
sis the number of taxa. For a 5-taxon tree, df = 5 - 2 = 3 [25] - Compare to critical value: The critical value for a chi-square distribution with 3 degrees of freedom at a significance level of α=0.05 is 7.82 [25]
- Conclusion: Since our test statistic (10.50) is greater than the critical value (7.82), we reject the null hypothesis. This indicates that the more complex model (without a molecular clock) fits the data significantly better, and the assumption of a homogeneous rate of evolution is not valid for this dataset [25].
Experimental Protocol for Model Comparison
This protocol outlines the key steps for performing a robust Likelihood Ratio Test.
- Define Nested Models: Clearly specify your null (H₀, simpler) and alternative (H₁, more complex) models. Ensure they are hierarchically nested [25].
- Compute Maximum Likelihood: Using your dataset, calculate the maximum likelihood estimates for the parameters of both models. Record the resulting maximum log-likelihood values (ℓ₀ and ℓ₁) [27].
- Calculate Test Statistic: Compute the LRT statistic using the formula: λ_LR = -2 * (ℓ₀ - ℓ₁) [26].
- Determine Degrees of Freedom: Calculate the degrees of freedom (df) as the difference in the number of free parameters between the two models [25].
- Significance Testing: Compare the λLR statistic to the critical value from the chi-square distribution with the calculated df at your chosen significance level (e.g., α = 0.05). If λLR exceeds the critical value, reject the null hypothesis in favor of the more complex model [25].
The logical workflow for this experimental protocol can be visualized as follows:
The Scientist's Toolkit: Essential Research Reagents
The following table lists key conceptual "reagents" and software tools essential for conducting Likelihood Ratio Test analysis.
| Tool/Concept | Function in LRT Analysis |
|---|---|
| Nested Models | A pair of models where the simpler one (H₀) is a special case of the complex one (H₁), created by constraining parameters. This is an imperative requirement for the LRT [25]. |
| Likelihood Function (L(θ)) | The function that expresses the probability of observing the collected data given a set of model parameters (θ). It is the core component from which likelihoods are calculated [28]. |
| Maximized Log-Likelihood (ℓ) | The natural logarithm of the maximum value of the likelihood function achieved after optimizing model parameters. Used directly in the LRT statistic calculation [26]. |
| Chi-Square Distribution (χ²) | The theoretical probability distribution used to determine the statistical significance of the LRT statistic under the null hypothesis, thanks to Wilk's Theorem [27]. |
| Statistical Software (R, etc.) | Platforms used to perform numerical optimization (maximizing likelihoods), compute the LRT statistic, and compare it to the chi-square distribution [27]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My LRT statistic is negative. Is this possible, and what does it mean?
A negative LRT statistic typically indicates an error in calculation. The LRT statistic is defined as λ_LR = -2 * (ℓ₀ - ℓ₁), where ℓ₁ is the log-likelihood of the more complex model. Because a model with more parameters will always fit the data at least as well as a simpler one, ℓ₁ should always be greater than or equal to ℓ₀. Therefore, (ℓ₀ - ℓ₁) should be zero or negative, making the full statistic zero or positive. A negative value suggests the log-likelihoods have been swapped in the formula [26].
Q2: Can I use the LRT to compare non-nested models? No, the standard Likelihood Ratio Test is only valid for comparing hierarchically nested models [25]. If your models are not nested (e.g., one uses a normal error distribution and another uses a gamma distribution), the LRT statistic may not follow a chi-square distribution. In such cases, you would need to use generalized methods like relative likelihood or information-theoretic criteria such as AIC (Akaike Information Criterion) for model comparison [26].
Q3: The LRT and the Wald test both seem to test model parameters. What is the difference? The LRT, the Wald test, and the Lagrange Multiplier test are three classical approaches that are asymptotically equivalent but operate differently. The key difference is that the LRT requires fitting both the null and alternative models, while the Wald test only requires fitting the more complex alternative model. The LRT is generally considered more reliable than the Wald test for smaller sample sizes, though it is computationally more intensive because both models must be estimated [26].
Q4: My sample size is relatively small. Should I be concerned about using the LRT? Yes, sample size is an important consideration. Wilk's Theorem, which states that the LRT statistic follows a chi-square distribution, is an asymptotic result. This means it holds as the sample size approaches infinity [27]. With small sample sizes, the actual distribution of the test statistic may not be well-approximated by the chi-square distribution, potentially leading to inaccurate p-values. In such situations, results should be interpreted with caution.
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: What is the primary challenge with unmeasured confounding in indirect treatment comparisons, and when is it most pronounced?
Unmeasured confounding is a major concern in indirect treatment comparisons (ITCs) and external control arm analyses where treatment assignment is non-random. This bias occurs when patient characteristics associated with both treatment selection and outcomes remain unaccounted for in the analysis. The problem is particularly pronounced when comparing therapies with differing mechanisms of action that lead to violation of the proportional hazards (PH) assumption, which is common in oncology immunotherapy studies and other time-to-event analyses. Traditional sensitivity analyses often fail in these scenarios because they rely on the PH assumption, creating an unmet need for more flexible quantitative bias analysis methods. [29] [30]
FAQ 2: My bias analysis results appear unstable with wide confidence intervals. What might be causing this?
This instability often stems from insufficient specification of confounder characteristics or inadequate handling of non-proportional hazards. The multiple imputation approach requires precise specification of the unmeasured confounder's relationship with both treatment and outcome. Ensure you have:
- Clearly defined hypothesized strength of association between confounder and treatment
- Well-specified relationship between confounder and outcome
- Appropriate handling of censoring in time-to-event data
- Sufficient number of imputations (typically 20+)
Additionally, when PH violation is present, using inappropriate effect measures like hazard ratios rather than difference in restricted mean survival time (dRMST) can introduce substantial bias and variability in results. [29] [30]
FAQ 3: How can I determine what strength of unmeasured confounding would nullify my study conclusions?
Implement a tipping point analysis using the following workflow:
- Specify a range of plausible associations between the unmeasured confounder and treatment, and between the confounder and outcome
- Use multiple imputation to create complete datasets adjusting for these specified relationships
- Calculate adjusted treatment effects (preferably dRMST under PH violation) for each scenario
- Identify the confounder strength where confidence intervals cross the null value
- Assess plausibility of identified confounder characteristics in your clinical context
This approach reveals how robust your conclusions are to potential unmeasured confounding and whether plausible unmeasured confounders could explain away your observed effects. [30]
FAQ 4: What are the key differences between delta-adjusted and multiple imputation methods for handling unmeasured confounding?
Table: Comparison of Delta-Adjusted and Multiple Imputation Methods
| Feature | Delta-Adjusted Methods | Multiple Imputation Methods |
|---|---|---|
| Implementation | Bias-formula based direct computation [30] | Simulation-based with Bayesian data augmentation [29] [30] |
| Flexibility | Limited to specific confounding scenarios [30] | High flexibility for various confounding types and distributions [29] [30] |
| PH Violation Handling | Generally requires PH assumption [30] | Valid under proportional hazards violation [29] [30] |
| Effect Measure | Typically hazard ratios [30] | Difference in restricted mean survival time (dRMST) [29] [30] |
| Ease of Use | Relatively straightforward implementation [30] | Requires advanced statistical expertise [30] |
| Output | Direct adjusted effect estimates [30] | Imputed confounder values for weighted analysis [29] [30] |
FAQ 5: How do I validate that my multiple imputation approach for unmeasured confounding is working correctly?
Validation should include both simulation studies and diagnostic checks:
- Perform simulation studies: Generate data with known confounding mechanisms and assess whether your imputation approach accurately recovers the true adjusted effect
- Check convergence: Monitor convergence of your Bayesian data augmentation algorithm
- Assess coverage: Verify that confidence intervals achieve nominal coverage rates
- Compare to full adjustment: When possible, compare results to analyses with all confounders measured
- Conduct sensitivity analyses: Test how results vary under different assumptions about the unmeasured confounder
Research shows that properly implemented imputation-based adjustment can estimate the true adjusted dRMST with minimal bias comparable to analyses with all confounders measured. [29] [30]
Experimental Protocols and Methodologies
Protocol 1: Multiple Imputation with Bayesian Data Augmentation for dRMST
Application: Adjusting for unmeasured confounding in time-to-event analyses with non-proportional hazards.
Step-by-Step Methodology:
Define Outcome and Propensity Models:
- Specify outcome model: (f\left({t}{i} | {z}{i}, {x}{i}, {u}{i},{\delta }{i},{\varvec{\theta}},{{\varvec{\beta}}}{x},{{\varvec{\beta}}}_{u}\right))
- Specify propensity model: (\text{logit}\left(p\left({z}{i}=1 | {x}{i}, {u}{i}\right)\right) = {a}{0} + {a}{x}^{T}{x}{i} + {a}{u}{u}{i})
- Where ({t}{i}) represents time-to-event, ({z}{i}) is treatment, ({x}{i}) are measured confounders, and ({u}{i}) is the unmeasured confounder [30]
Specify Confounder Characteristics:
- Define hypothesized prevalence of binary unmeasured confounder
- Specify association between confounder and treatment (({a}_{u}))
- Specify association between confounder and outcome (({{\varvec{\beta}}}_{u}))
Implement Bayesian Data Augmentation:
- Use Markov Chain Monte Carlo (MCMC) methods for multiple imputation
- Iterate between imputing missing confounder values and updating model parameters
- Generate multiple complete datasets (typically 20+ imputations)
Perform Adjusted Analysis:
- Calculate dRMST for each imputed dataset
- Use appropriate weighting schemes for confounder adjustment
- Account for censoring in time-to-event data
Pool Results:
Protocol 2: Tipping Point Analysis for Unmeasured Confounding
Application: Determining the strength of unmeasured confounding required to nullify study conclusions.
Step-by-Step Methodology:
Define Parameter Grid:
- Create a systematic grid of plausible values for confounder-treatment association (({a}_{u}))
- Create a systematic grid of plausible values for confounder-outcome association (({{\varvec{\beta}}}_{u}))
- Range should cover clinically realistic scenarios
Iterative Adjustment:
- For each combination of (({a}{u}), ({{\varvec{\beta}}}{u})) in the parameter grid:
- Implement multiple imputation as in Protocol 1
- Calculate adjusted dRMST and confidence intervals
- Store results for each parameter combination
- For each combination of (({a}{u}), ({{\varvec{\beta}}}{u})) in the parameter grid:
Identify Tipping Points:
- Determine the parameter combinations where confidence intervals for dRMST include the null value
- Identify the minimum confounder strength that would nullify findings
- Create contour plots or similar visualizations to display results
Interpret Clinical Relevance:
- Assess whether identified confounder characteristics are plausible in your clinical context
- Determine robustness of study conclusions to potential unmeasured confounding [30]
Experimental Workflow and Signaling Pathways
Multiple Imputation QBA Workflow
Statistical Relationships in Sensitivity Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Methodological Components for Unmeasured Confounding Analysis
| Component | Function | Implementation Considerations |
|---|---|---|
| Bayesian Data Augmentation | Multiple imputation of unmeasured confounders using MCMC methods | Requires specification of prior distributions; computationally intensive but flexible [29] [30] |
| Restricted Mean Survival Time (RMST) | Valid effect measure under non-proportional hazards | Requires pre-specified time horizon; provides interpretable difference in mean survival [29] [30] |
| Tipping Point Analysis Framework | Identifies confounder strength needed to nullify results | Systematically varies confounder associations; produces interpretable sensitivity bounds [30] |
| Propensity Score Integration | Balances measured covariates in observational studies | Can be combined with multiple imputation for comprehensive adjustment [31] |
| Simulation-Based Validation | Assesses operating characteristics of methods | Verifies Type I error control, power, and coverage rates [29] [30] |
Frequently Asked Questions (FAQs)
Q1: What is the core advantage of using LRT methods over traditional meta-analysis for drug safety signal detection? Traditional meta-analysis often focuses on combining study-level summary measures (e.g., risk ratio) for a single, pre-specified adverse event (AE). In contrast, the LRT-based methods are designed for the simultaneous screening of many drug-AE combinations across multiple studies, thereby controlling the family-wise type I error and false discovery rates, which is crucial when exploring large safety databases [32] [33] [34].
Q2: How do the LRT methods handle the common issue of heterogeneous data across different studies? The LRT framework offers variations specifically designed to address heterogeneity. The simple pooled LRT method combines data across studies, while the weighted LRT method incorporates total drug exposure information by study, assigning different weights to account for variations in sample size or exposure. Simulation studies have shown these methods maintain performance even with varying heterogeneity across studies [32] [33].
Q3: My data includes studies with different drug exposure times. Is the standard LRT method still appropriate?
The standard LRT method for passive surveillance databases like FAERS uses reporting counts (e.g., n_i.) as a proxy for exposure. However, when actual exposure data (e.g., patient-years, P_i) is available from clinical trials, the model can be adapted to use these exposure-adjusted measures. Using unadjusted incidence percentages when exposure times differ can lead to inaccurate interpretations, and an exposure-adjusted model is more appropriate [33] [35].
Q4: A known problem in meta-analysis is incomplete reporting of adverse events, especially rare ones. Can LRT methods handle this? Standard LRT methods applied to summary-level data may be susceptible to bias from censored or unreported AEs. While the core LRT methods discussed here do not directly address this, recent statistical research has proposed Bayesian approaches to specifically handle meta-analysis of censored AEs. These methods can improve the accuracy of incidence rate estimations when such reporting issues are present [36].
Troubleshooting Common Experimental Issues
Problem: Inconsistent or Missing Drug Exposure Data Across Studies
Issue: The definition and availability of total drug exposure (P_i) may vary or be missing in some studies, making the weighted LRT method difficult to apply.
Solution:
- Imputation with Assumptions: If precise exposure is not collected, it may be imputed using reasonable assumptions based on available data, such as study duration and dosage information [33].
- Standardized Protocols: Ensure future studies adhere to a standardized protocol for collecting and reporting exposure data to ensure consistency [33].
- Sensitivity Analysis: Conduct analyses using both the simple pooled LRT (without exposure data) and the weighted LRT (with imputed data) to assess the robustness of your findings.
Problem: High False Discovery Rate (FDR) When Screening Hundreds of AEs Issue: Simultaneously testing multiple drug-AE combinations increases the chance of false positives. Solution:
- Utilize LRT's Inherent Properties: The LRT method was developed to control the family-wise type I error and FDR. Ensure you are using the maximum likelihood ratio (MLR) test statistic and the correct critical values from the derived distribution [34].
- Confirm with External Evidence: Signals detected by the statistical method should be confirmed by existing medical evidence, biological plausibility, or signals from other independent databases [34].
Problem: Integrating Data from Studies with Different Designs (e.g., RCTs and Observational Studies) Issue: Simple pooling of AE data from studies with different designs can lead to confounding and inaccurate summaries. Solution:
- Stratified Analysis: Use a meta-analytic approach that stratifies by trial or study type to preserve the randomization of RCTs and account for design differences. A valid meta-analysis should feature appropriate adjustments and weights for distinct trials [35].
- Bayesian Hierarchical Models: Consider advanced models that add a layer for the clinical trial level, which can borrow information across studies while accounting for their differences [35].
Key Experimental Protocols & Data Presentation
Core Protocol: Applying LRT Methods for Signal Detection
The following workflow outlines the standard methodology for applying LRT methods to multiple datasets for safety signal detection [32] [33].
The table below summarizes the three primary LRT approaches for multiple studies, as identified in the literature.
Table 1: Overview of LRT Methods for Drug Safety Signal Detection in Multiple Studies
| Method Name | Description | Key Formula/Statistic | When to Use |
|---|---|---|---|
| Simple Pooled LRT | Data from multiple studies are pooled together into a single 2x2 table for analysis [32] [33]. | LR_ij = [ (n_ij / E_ij)^n_ij * ( (n_.j - n_ij) / (n_.j - E_ij) )^(n_.j - n_ij) ] / [ (n_.j / n..)^n_.j ] [33] |
Initial screening when study heterogeneity is low and drug exposure data is unavailable or inconsistent. |
| Weighted LRT | Incorporates total drug exposure information (P_i) by study, giving different weights to studies [32] [33]. |
Replaces n_i. with P_i and n.. with P. in the calculation of E_ij and the LR statistic [33]. |
Preferred when reliable drug exposure data (e.g., patient-years) is available and comparable across all studies. |
| Two-Step LRT | Applies the regular LRT to each study individually, then combines the test statistics from different studies for a global test [33]. | Step 1: Calculate LRT statistic per study. Step 2: Combine statistics (e.g., by summing) for a global test [33]. | Useful for preserving study identity and assessing heterogeneity before combining results. |
Applied Example: Protocol for Analyzing PPIs and Osteoporosis
For illustration, one applied study analyzed the effect of concomitant use of Proton Pump Inhibitors (PPIs) in patients being treated for osteoporosis, using data from 6 studies [32] [33].
Experimental Protocol:
- Data Extraction: For each of the 6 studies, identify patients in two groups: those taking PPI + osteoporosis drug (active group) and those taking placebo + osteoporosis drug (control group).
- Outcome Definition: Identify all reported adverse events of interest from the safety data.
- Contingency Table Construction: For each study and each AE, construct a 2x2 contingency table with the counts for the drug group and the control group.
- Analysis: Apply the chosen LRT method (e.g., weighted LRT if exposure data is available) to the combined data from the 6 studies to test for a global safety signal associated with PPIs.
Table 2: Key Resources for Conducting LRT-based Safety Meta-Analyses
| Category | Item / Method | Function / Description | Key Reference / Source |
|---|---|---|---|
| Statistical Methods | Likelihood Ratio Test (LRT) | Core statistical test for identifying disproportionate reporting in 2x2 tables. | [32] [34] |
| Bayesian Hierarchical Model | An alternative/complementary method that accounts for data hierarchy and borrows strength across studies or AE terms. | [35] | |
| Proportional Reporting Ratio (PRR) | A simpler disproportionality method often used for benchmark comparison. | [33] [37] | |
| Data Sources | FDA Adverse Event Reporting System (FAERS) | A primary spontaneous reporting database for post-market safety surveillance. | [33] [37] [34] |
| EudraVigilance | The European system for managing and analyzing reports of suspected AEs. | [37] | |
| Clinical Trial Databases | Aggregated safety data from multiple pre-market clinical trials for a drug. | [32] [35] | |
| Software & Tools | OpenFDA | Provides interactive, open-source applications for data mining and visualization of FAERS data. | [33] [37] |
| R / SAS | Standard statistical software environments capable of implementing custom LRT and meta-analysis code. | (Implied) |
Frequently Asked Questions (FAQs)
FAQ 1: What is the most structured method to handle missing data that is suspected to be Not Missing at Random (NMAR) in time-to-event analysis?
The Delta-Adjusted Multiple Imputation (DA-MI) approach is a highly structured method for handling NMAR data in time-to-event analyses. Unlike traditional methods that rely on pattern-mixture or selection models without direct imputation, DA-MI explicitly adjusts imputed values using sensitivity parameters (delta shifts (δ)) within a Multiple Imputation framework [17] [38]. This provides a structured way to handle deviations from the Missing at Random (MAR) assumption. It works by generating multiple datasets with controlled sensitivity adjustments, which preserves the relationship between time-dependent covariates and the event-time outcome while accounting for intra-individual variability [17]. The results offer sensitivity bounds for treatment effects under different missing data scenarios, making them highly interpretable for decision-making [17] [38].
FAQ 2: My primary analysis assumes data is Missing at Random (MAR). How can I test the robustness of my conclusions?
Conducting a sensitivity analysis is essential. Your primary analysis under MAR should be supplemented with sensitivity analyses that explore plausible NMAR scenarios [39]. The Delta-Adjusted method is perfectly suited for this. You would:
- Start with your MAR-based imputation.
- Create multiple versions of your imputed dataset by systematically applying different delta (δ) values to the imputed missing data. These delta values represent specified deviations from the MAR assumption [17] [39].
- Analyze each of these adjusted datasets and combine the results.
- Observe how your estimated treatment effect changes across the different delta values. If your conclusions remain unchanged under a range of plausible NMAR scenarios, your results are considered robust [17].
FAQ 3: What is a "Tipping Point Analysis" for missing data in clinical trials with time-to-event endpoints?
A Tipping Point Analysis is a specific type of sensitivity analysis that aims to find the critical degree of deviation from the primary analysis's missing data assumptions at which the trial's conclusion changes (e.g., from significant to non-significant) [40]. This approach can be broadly categorized into:
- Model-Based Approaches: These involve varying parameters within a statistical model used to handle missing data.
- Model-Free Approaches: These are less emphasized in literature but offer alternative ways to impute missing data and assess robustness [40]. The goal is to evaluate how much the missing data mechanism would need to differ from the MAR assumption to alter the trial's primary outcome, thus providing a practical measure of result reliability [40].
FAQ 4: When should I use a global sensitivity analysis instead of a local one?
You should prefer global sensitivity analysis for any model that cannot be proven linear. Local sensitivity analysis, which varies parameters one-at-a-time around specific reference values, has critical limitations [41]:
- It can be heavily biased for nonlinear models.
- It underestimates the importance of factors that interact.
- It only partially explores the model's parametric space [41]. In contrast, global sensitivity analysis varies all uncertain factors simultaneously across their entire feasible space. This reveals the global effects of each parameter on the model output, including any interactive effects, leading to a more comprehensive understanding of your model's behavior [41].
Troubleshooting Guides
Problem: My time-to-event analysis has missing time-dependent covariates, and I suspect the missingness is related to a patient's unobserved health status (NMAR).
Solution: Implement a Delta-Adjusted Multiple Imputation (DA-MI) workflow.
| Step | Action | Key Consideration |
|---|---|---|
| 1 | Specify the MAR Imputation Model | Use Multiple Imputation by Chained Equations (MICE) to impute missing values under the MAR assumption. Ensure the imputation model includes the event indicator, event/censoring time, and other relevant covariates [17] [39]. |
| 2 | Define Delta (δ) Adjustment Scenarios | Choose a range of delta values that represent plausible NMAR mechanisms. For example, a positive δ could increase the imputed value of a covariate for missing cases, assuming that missingness is linked to poorer health [17]. |
| 3 | Generate Adjusted Datasets | Create multiple copies of the imputed dataset, applying the predefined δ adjustments to the imputed values for missing observations [17]. |
| 4 | Analyze and Combine Results | Fit your time-to-event model (e.g., Cox regression) to each adjusted dataset. Pool the results using Rubin's rules to obtain estimates and confidence intervals for each NMAR scenario [17]. |
| 5 | Interpret Sensitivity Bounds | Compare the pooled treatment effects across different δ values. The range of results shows how sensitive your findings are to departures from the MAR assumption [17] [38]. |
Problem: I am unsure which uncertain inputs in my computational model have the most influence on the time-to-event output.
Solution: Perform a global sensitivity analysis for factor prioritization.
| Step | Action | Objective |
|---|---|---|
| 1 | Define Uncertainty Space | Identify all model parameters, inputs, and structures considered uncertain. Define plausible ranges for each based on literature, expert opinion, or observed data [41]. |
| 2 | Generate Input Samples | Use a sampling method (e.g., Monte Carlo, Latin Hypercube) to generate a large number of input vectors that cover the entire defined uncertainty space [41]. |
| 3 | Run Model & Compute Output | Execute your time-to-event model for each input vector and record the output metric of interest (e.g., estimated hazard ratio) [41]. |
| 4 | Calculate Sensitivity Indices | Compute variance-based sensitivity indices (e.g., Sobol' indices). The first-order index measures the individual contribution of an input to the output variance, while the total-order index includes interaction effects [41]. |
| 5 | Prioritize Factors | Rank the inputs based on their sensitivity indices. Inputs with the highest indices are the most influential and should be prioritized for further measurement or refinement to reduce output uncertainty [41]. |
Experimental Protocols
Protocol: Conducting a Delta-Adjusted MI Sensitivity Analysis for a Cox Proportional Hazards Model
Objective: To assess the robustness of a treatment effect estimate from a Cox model to NMAR assumptions regarding missing time-dependent covariates.
Materials and Dataset:
- Dataset: A time-to-event dataset (e.g., time-to-tumor progression in a prostate cancer study) with two or more time-dependent covariates containing missing observations [17].
- Software: Statistical software capable of performing multiple imputation (e.g., R, Stata, SAS).
Procedure:
- Preliminary Analysis: Perform a Complete Case Analysis (CCA) to get a preliminary estimate under the likely incorrect MCAR assumption [17].
- MAR-Based MI: Use the MICE algorithm to create
m(e.g., 20) complete datasets, imputing under the MAR assumption. The imputation model must include the event time, event indicator, and other relevant covariates [17]. - Define NMAR Scenarios: Convene subject-matter experts to define a set of
kplausible delta (δ) values. For example, for a biomarker, δ could be+0.5,+1.0, and+1.5standard deviations, representing scenarios where missing values are systematically higher [17]. - Apply Delta Adjustment: For each of the
mMAR-imputed datasets, createkadjusted versions by adding the δ value to the imputed values for the specified covariate(s). - Model Fitting: Fit the Cox proportional hazards model to each of the
m x kfinal datasets. - Result Pooling: Use Rubin's rules to pool the
mresults within each of thekNMAR scenarios. This will yieldkpooled Hazard Ratios (HRs) and confidence intervals.
Diagram 1: DA-MI analysis workflow for NMAR data.
Protocol: Performing a Tipping Point Analysis for a Time-to-Event Endpoint
Objective: To determine the degree of deviation from the primary analysis's missing data assumptions required to change the trial's conclusion (e.g., statistical significance of a treatment effect).
Materials:
- Dataset: Clinical trial data with a time-to-event primary endpoint where some events are censored due to dropouts or loss to follow-up [40].
- Software: Statistical software with capabilities for tipping point analysis (e.g., R with appropriate packages).
Procedure:
- Primary Analysis: Conduct your pre-specified primary analysis (e.g., Cox model assuming censoring at random) to establish the base treatment effect and p-value.
- Select Tipping Point Method: Choose either a model-based (e.g., using pattern-mixture models) or model-free approach (e.g., direct imputation of event times for censored cases) for the analysis [40].
- Define Tipping Condition: Clearly state the condition that defines a "tip," such as the pooled Hazard Ratio (HR) becoming greater than 1.0 or the p-value exceeding 0.05.
- Systematic Variation: Systematically vary the key sensitivity parameter in your chosen method. In a model-free approach, this could involve imputing increasingly divergent event times for the censored subjects in the treatment group versus the control group.
- Identify Tipping Point: Run the analysis at each level of variation. The tipping point is the smallest degree of variation at which the pre-defined tipping condition is met.
- Plausibility Assessment: In collaboration with clinical experts, assess whether the identified tipping scenario is clinically plausible. If the required deviation is implausibly large, the primary result is considered robust [40].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Methodological Components for Sensitivity Analysis
| Item | Function & Application |
|---|---|
| Multiple Imputation by Chained Equations (MICE) | A flexible framework for handling missing data by creating multiple plausible datasets. It is the foundation for implementing more advanced methods like Delta-Adjustment [17] [39]. |
| Delta (δ) Parameter | A sensitivity parameter used to shift imputed values in a controlled manner. It quantifies the postulated deviation from the MAR assumption, allowing for structured NMAR sensitivity analysis [17] [39]. |
| Cox Proportional Hazards Model | The standard regression model for analyzing the effect of covariates on time-to-event data. It is the typical "substantive model" used after imputation to estimate treatment effects [17] [42]. |
| Rubin's Rules | The standard set of formulas for combining parameter estimates and standard errors from multiple imputed datasets. They ensure valid statistical inference that accounts for imputation uncertainty [17]. |
| Variance-Based Sensitivity Indices (e.g., Sobol') | Quantitative measures from global sensitivity analysis used for factor prioritization. They apportion the variance in the model output to different input factors, both individually and through interactions [41]. |
| Tipping Point Condition | A pre-specified criterion (e.g., HR=1, p=0.05) used to judge when the conclusion of a study changes. It is the target for identifying the critical assumption in a tipping point analysis [40]. |
Frequently Asked Questions (FAQs)
1. What is the primary purpose of sensitivity analysis in pharmacoepidemiology studies? Sensitivity analysis determines the robustness of research findings by examining how results are affected by changes in methods, models, values of unmeasured variables, or assumptions [8]. It helps identify which results are most dependent on questionable or unsupported assumptions, thereby assessing the credibility of a study's conclusions [43] [44].
2. How often do sensitivity analyses actually change the conclusions of a study? A systematic review found that 54.2% of observational studies showed significant differences between primary and sensitivity analyses, with an average difference in effect size of 24% [43]. Despite this, only a small fraction of these studies (9 out of 71) discussed the potential impact of these inconsistencies, indicating that differences are rarely taken into account in final interpretations [43].
3. What are the main categories of sensitivity analyses? Following Agency for Healthcare Research and Quality (AHRQ) guidance, sensitivity analyses in observational comparative effectiveness research are typically categorized into three main dimensions [43] [44]:
- Alternative Study Definitions: Modifying exposure, outcome, or confounder definitions
- Alternative Study Designs: Changing the data source or population under study
- Alternative Modeling: Modifying statistical approaches or handling of missing data
4. When should I consider using a likelihood ratio model for exposure classification? Likelihood ratio models are particularly valuable when working with prescription databases where actual treatment duration after redeeming a prescription is not recorded. These models can reduce misclassification bias compared to traditional decision rules, which often force a false dichotomy on exposure status [45].
5. What are common factors that lead to inconsistent results between primary and sensitivity analyses? Multivariable regression has identified that conducting three or more sensitivity analyses, not having a large effect size, using blank controls, and publishing in a non-Q1 journal were all more likely to exhibit inconsistent results between primary and sensitivity analyses [43].
Troubleshooting Guides
Problem: Inconsistent Results Between Primary and Sensitivity Analyses
Symptoms:
- Point estimates or confidence intervals meaningfully change across analyses
- Statistical significance appears or disappears
- Effect direction reverses
Diagnostic Steps:
- Categorize the Inconsistency: Determine whether discrepancies stem from alternative study definitions, designs, or statistical models [43].
- Check Effect Size Magnitude: Note that studies without large effect sizes (0.5-2 for ratio measures) are more prone to inconsistencies [43].
- Review Control Group Selection: Blank controls (vs. active comparators) show higher rates of inconsistency [43].
Resolution Strategies:
- Systematic Documentation: Create a matrix comparing all analyses and their results
- Prioritize Plausibility: Favor assumptions and definitions with strongest clinical or epidemiological justification
- Quantitative Bias Analysis: Implement formal methods to estimate potential impact of unmeasured confounding [46]
- Transparent Reporting: Clearly discuss all inconsistencies and their potential implications in publications [43]
Problem: Implementing the Reverse Waiting Time Distribution Model
Symptoms:
- Exposure misclassification persists despite sophisticated methods
- Model convergence issues
- Parameter estimates with poor precision
Diagnostic Steps:
- Verify Data Structure: Ensure prescription redemption data includes exact dates and appropriate observation windows [45]
- Check Model Specification: Confirm the parametric reverse WTD model properly fits the last observed prescription redemption among controls [45]
- Assess Misspecification Impact: Evaluate whether moderate model misspecification substantially affects results [45]
Resolution Strategies:
- Joint Likelihood Implementation: Use the joint likelihood model that incorporates both latent exposure status and exposure-outcome association for consistency and efficiency [45]
- Validation Checks: Compare results with standard decision-rule based analyses to identify substantial discrepancies [45]
- Covariate Adjustment: Include relevant covariates in both parts of the likelihood model to adjust for observed confounders [45]
Problem: Handling Unmeasured Confounding in Sensitivity Analyses
Symptoms:
- Residual confounding suspected despite comprehensive adjustment
- Unexplained differences between studies of same research question
- Concerns about confounding by indication
Diagnostic Steps:
- Assess Confounding Direction: Determine whether unmeasured confounding would likely bias results toward or away from the null
- Evaluate E-Values: Calculate the minimum strength of association an unmeasured confounder would need to have to explain away the observed effect [43]
- Review Control Outcomes: Implement negative control outcomes to detect residual confounding [46]
Resolution Strategies:
- Quantitative Bias Analysis: Implement methods that can estimate study results in the presence of a hypothesized unmeasured confounder [44]
- Multiple Comparison Groups: Include several different comparison groups and use observed differences in potential biases as a way to assess robustness [44]
- Quasi-Experimental Methods: Consider instrumental variable analysis or other approaches that account for unmeasured confounding [44]
Table 1: Frequency and Impact of Sensitivity Analyses in Observational Studies (n=256) [43]
| Metric | Value | Implication |
|---|---|---|
| Studies conducting sensitivity analyses | 152 (59.4%) | Underutilization in ~40% of studies |
| Median number of sensitivity analyses per study | 3 (IQR: 2-6) | Multiple tests common when used |
| Studies with clearly reported results | 131 (51.2%) | Reporting transparency needs improvement |
| Studies with significant primary vs. sensitivity analysis differences | 71 (54.2%) | Inconsistencies frequent but often unaddressed |
| Average difference in effect size | 24% (95% CI: 12-35%) | Substantial quantitative impact |
Table 2: Types of Sensitivity Analyses Showing Inconsistencies (n=145) [43]
| Analysis Type | Frequency | Common Examples |
|---|---|---|
| Alternative study definitions | 59 (40.7%) | Varying exposure, outcome, or confounder algorithms |
| Alternative study designs | 39 (26.9%) | Changing data source, inclusion periods |
| Alternative statistical models | 38 (26.2%) | Different handling of missing data, model specifications |
| Other | 9 (6.2%) | E-values, unmeasured confounding assessments |
Table 3: Performance Comparison of Exposure Classification Methods [45]
| Method | Relative Bias | Coverage Probability | Empirical Example: NSAID-UGIB OR |
|---|---|---|---|
| New joint likelihood model | <1.4% | 90.2-95.1% | 2.52 (1.59-3.45) |
| Standard decision-rule methods | -21.1 to 17.0% | 0.0-68.9% | 3.52-5.17 (range across methods) |
Experimental Protocols
Protocol 1: Implementing a Comprehensive Sensitivity Analysis Plan
Background: Following Good Pharmacoepidemiology Practices (GPP), every study should include a protocol describing planned sensitivity analyses to assess robustness [47].
Materials:
- Primary analysis specification
- Directed Acyclic Graphs (DAGs) identifying potential sources of bias
- Statistical analysis plan with pre-specified variations
Procedure:
- Pre-specification: Document all planned sensitivity analyses in the study protocol before conducting primary analysis [47]
- Three-Dimensional Approach:
- Implementation:
- Execute all pre-specified analyses identically to primary analysis except for the varied element
- Document any computational or convergence issues
- Interpretation Framework:
- Compare point estimates, confidence intervals, and statistical significance across analyses
- Assess whether conclusions would change substantively under different assumptions
- Report all results regardless of consistency [43]
Validation:
- Follow ISPE GPP guidelines for quality assurance [47]
- Use version-controlled statistical code to ensure reproducibility
- Apply sensitivity analyses uniformly across all primary outcomes
Protocol 2: Applying the Reverse Waiting Time Distribution Model
Background: The reverse Waiting Time Distribution approach estimates latent exposure status from prescription redemption data, reducing misclassification bias compared to traditional decision rules [45].
Materials:
- Database with individual prescription redemption records
- Case-control status indicator
- Dates of last prescription redemption before index date
- Covariate data for adjustment
Procedure:
- Data Preparation:
- For each case and control, calculate time R from last prescription redemption to index date
- Create indicator V for whether any redemption occurred in predefined window before index date
- Exclude individuals with no redemptions in observation period (assumed unexposed) [45]
Model Specification:
- Establish joint likelihood combining reverse WTD and logistic regression components
- Model the backward recurrence time (R) as originating from a renewal process
- Incorporate case-control status (Y) depending on latent exposure status (Z) via logistic model: P(Y=1|Z=z) = exp(β₀ + β₁z) / [1 + exp(β₀ + β₁z)] [45]
Parameter Estimation:
- Maximize the joint likelihood to obtain estimates for both exposure distribution and exposure-outcome association parameters
- Include relevant covariates in both likelihood components to adjust for confounding
- Use maximum likelihood estimation with appropriate numerical methods [45]
Model Checking:
- Compare results with standard decision-rule based analyses
- Assess model fit using appropriate goodness-of-fit measures
- Conduct simulation studies if possible to evaluate potential misspecification [45]
Validation:
- Compare results with external validation data when available
- Assess sensitivity to model assumptions through misspecification analyses
- Verify that confidence intervals maintain nominal coverage probabilities [45]
Experimental Workflow Visualization
Sensitivity Analysis Implementation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Methodological Tools for Sensitivity Analysis in Pharmacoepidemiology
| Tool/Technique | Function | Application Context |
|---|---|---|
| Directed Acyclic Graphs (DAGs) | Visual representation of causal assumptions and potential biases | Identifying potential confounders and sources of bias during study design [46] |
| E-Value Calculation | Quantifies minimum strength of unmeasured confounding needed to explain away effect | Assessing robustness to unmeasured confounding [43] |
| Reverse Waiting Time Distribution | Models latent exposure status from prescription redemption patterns | Reducing exposure misclassification in pharmacoepidemiology studies [45] |
| Negative Control Outcomes | Uses outcomes not causally related to exposure to detect residual confounding | Detecting unmeasured confounding and other biases [46] |
| Multiple Comparison Groups | Tests robustness across different control selection strategies | Assessing impact of comparator choice on effect estimates [44] |
| Quantitative Bias Analysis | Formal methods to quantify potential impact of specific biases | Estimating how much biases might affect observed results [46] |
Navigating Challenges: Ensuring Reliability and Optimizing LR Model Performance
Frequently Asked Questions (FAQs)
Q1: What is model misspecification in the context of sensitivity analysis for likelihood ratio models? Model misspecification occurs when your econometric or statistical model fails to capture the true relationship between dependent and independent variables. In likelihood ratio models, this means your model may not accurately represent the underlying data-generating process, potentially leading to biased estimates and incorrect conclusions in your sensitivity analysis. Common types include omitted variables, incorrect functional form, and measurement errors [48].
Q2: How do high-variance estimates affect the reliability of drug development research? High-variance estimates indicate that your model's predictions change substantially when trained on different data subsets. In drug development, this overfitting problem means your results may not generalize beyond your specific sample, potentially leading to unreliable clinical trial outcomes, inefficient resource allocation, and compromised decision-making about treatment efficacy [49].
Q3: What are the most effective methods to detect model misspecification? Two primary approaches exist for detecting misspecification. Residual analysis examines patterns in the differences between actual and predicted values, where non-random patterns suggest potential issues. Formal specification tests include the Ramsey RESET test for omitted variables or incorrect functional form, Breusch-Pagan test for heteroskedasticity, and Durbin-Watson test for autocorrelation [48].
Q4: Why does including too many covariates lead to high variance? Adding excessive covariates increases model complexity and provides more degrees of freedom to fit noise in the training data. While this may appear to improve fit (lower bias), it actually causes overfitting where the model becomes overly sensitive to minor fluctuations in the training data, resulting in poor generalization to new data and high prediction variance [50].
Q5: How can researchers balance the bias-variance tradeoff in likelihood ratio models? The bias-variance tradeoff describes the conflict between minimizing two error sources: bias from overly simplistic models and variance from overly complex ones. Balancing this tradeoff involves selecting appropriate model complexity that captures true patterns without fitting noise, often through regularization, cross-validation, and ensemble methods [51].
Q6: What procedural steps can mitigate common method variance (CMV) in experimental research? CMV mitigation begins with research design rather than statistical corrections. Effective approaches include using multiple data sources, incorporating additional independent variables to distribute shared error variance, improving measurement reliability, and implementing temporal separation between measurements. Statistical controls like marker variables or latent methods should complement rather than replace design-based approaches [52].
Troubleshooting Guides
Diagnosing Model Misspecification
Symptoms:
- Biased parameter estimates that systematically deviate from true values
- Inefficient estimates with larger than expected variances
- Invalid hypothesis tests with incorrect p-values
- Inaccurate predictions that deviate substantially from actual values [48]
Diagnostic Steps:
Diagram: Model Misspecification Diagnostic Workflow
Corrective Actions:
- For omitted variables: Include theoretically relevant variables or use proxy variables
- For incorrect functional form: Apply transformations or use non-linear terms
- For measurement errors: Implement instrumental variables approaches
- For heteroskedasticity: Use robust standard errors or weighted estimation [48]
Addressing High-Variance Estimates
Symptoms:
- Excellent performance on training data but poor performance on test data
- Model predictions vary significantly with small changes in training data
- Large confidence intervals around parameter estimates
- Unstable model coefficients across different samples [49]
Diagnostic Steps:
Diagram: High-Variance Diagnostic Process
Mitigation Strategies:
- Apply regularization techniques (L1/Lasso or L2/Ridge)
- Implement ensemble methods like bagging or random forests
- Use dimensionality reduction (PCA) or feature selection
- Increase sample size where feasible
- Employ early stopping in iterative models [49]
Quantitative Reference Tables
Model Misspecification Types and Consequences
Table: Common Model Misspecification Types and Impacts
| Misspecification Type | Primary Consequences | Detection Methods | Correction Approaches |
|---|---|---|---|
| Omitted Variables | Biased coefficient estimates, Invalid hypothesis tests | Ramsey RESET test, Theoretical rationale | Include relevant variables, Instrumental variables [48] |
| Irrelevant Variables | Inefficient estimates, Reduced statistical power | t-tests/F-tests, Model selection criteria | Stepwise regression, Information criteria [48] |
| Incorrect Functional Form | Biased and inconsistent estimates | Residual plots, Rainbow test | Variable transformation, Nonlinear terms [48] |
| Measurement Error | Attenuation bias (bias toward zero) | Reliability analysis, Multiple indicators | Instrumental variables, Latent variable models [48] |
| Common Method Variance | Inflated relationships between variables | Marker variable tests, Procedural remedies | Design improvements, Statistical controls [52] |
Variance Reduction Technique Selection Guide
Table: Variance Reduction Techniques by Scenario
| Technique | Best For Model Types | Data Conditions | Implementation Complexity | Key Benefits |
|---|---|---|---|---|
| Cross-Validation | All models, especially complex ones | Limited data, Unseen data prediction | Medium | Reliable performance estimation [49] |
| Bagging (Bootstrap Aggregating) | Decision trees, Random forests | Small to medium datasets | Low-Medium | Reduces variance, Handles nonlinearity [49] |
| Regularization (L1/L2) | Linear models, Neural networks | High-dimensional data, Multicollinearity | Low | Prevents overfitting, Feature selection (L1) [49] |
| Pruning | Decision trees, Rule-based models | Noisy data, Complex trees | Medium | Improves interpretability, Reduces complexity [49] |
| Early Stopping | Neural networks, Gradient boosting | Large datasets, Iterative training | Low | Prevents overfitting, Saves computation [49] |
| Ensemble Methods | Multiple model combinations | Diverse data patterns, Competitions | High | Maximizes performance, Balances errors [49] |
| Feature Selection | High-dimensional problems | Many irrelevant features | Medium | Improves interpretability, Reduces noise [49] |
Experimental Protocols
Protocol for Detecting Common Method Variance
Purpose: Identify and quantify common method variance in Likelihood Ratio Models using sensitivity analysis.
Materials:
- Dataset with multiple measurement items
- Statistical software (R, Python, or specialized SEM tools)
- Marker variables (theoretically unrelated constructs)
Procedure:
- Measurement Design Phase
- Incorporate procedural remedies by varying scale types and endpoints
- Separate measurement of predictor and criterion variables temporally
- Include multiple independent variables to distribute shared error variance [52]
Statistical Control Implementation
- Apply the Unmeasured Latent Method Construct (ULMC) approach in SEM
- Use confirmatory factor analysis with marker variables
- Estimate model parameters with and without method factor
Sensitivity Analysis
- Compare parameter estimates across different CMV adjustment methods
- Assess stability of significance conclusions across specifications
- Calculate the impact of CMV on effect sizes and confidence intervals
Interpretation Guidelines
- Focus on consistency of statistical significance (Type I/II error rates)
- Evaluate whether conclusions change after CMV adjustments
- Report both adjusted and unadjusted estimates for transparency [52]
Protocol for Bias-Variance Tradeoff Optimization
Purpose: Systematically balance bias and variance in Likelihood Ratio Models for robust sensitivity analysis.
Materials:
- Training and testing datasets
- Cross-validation framework
- Regularization implementation
Procedure:
- Baseline Model Establishment
- Fit an initial model with theoretically justified complexity
- Record training and test performance metrics
- Calculate bias and variance decomposition
Complexity Variation Phase
- Systematically increase model complexity (add parameters, interactions)
- Decrease model complexity (remove terms, increase regularization)
- Track training and test error at each complexity level
Tradeoff Optimization
- Identify complexity level where test error is minimized
- Ensure sufficient gap between training and test performance
- Verify robustness through cross-validation
Validation and Sensitivity Reporting
- Document the selected model's bias-variance characteristics
- Report sensitivity of conclusions to different complexity choices
- Provide justification for final model selection based on tradeoff analysis [51]
Research Reagent Solutions
Table: Essential Methodological Tools for Sensitivity Analysis
| Research Tool | Primary Function | Application Context | Implementation Considerations |
|---|---|---|---|
| Likelihood Ratio Test | Model comparison, Nested model testing | Sensitivity analysis, Model specification checks | Requires nested models, Asymptotically χ² distributed |
| Regularization Parameters | Bias-variance control, Overfitting prevention | High-dimensional models, Multicollinearity | λ selection via cross-validation, Different L1/L2 penalties [49] |
| Cross-Validation Framework | Performance estimation, Hyperparameter tuning | Model selection, Variance reduction | k-fold design, Stratified sampling for classification [49] |
| Instrumental Variables | Endogeneity correction, Omitted variable bias | Causal inference, Measurement error | Exclusion restriction validity, Weak instrument tests [48] |
| Specification Tests | Misspecification detection, Functional form checks | Model validation, Assumption verification | RESET test, Heteroskedasticity tests, Normality tests [48] |
| Ensemble Methods | Variance reduction, Prediction improvement | Complex patterns, Multiple data types | Computational intensity, Interpretation challenges [49] |
| Marker Variables | Common method variance assessment | Survey research, Self-report data | Theoretical justification, Measurement equivalence [52] |
Troubleshooting Guide: Data Integrity in Research
Q1: My dataset has extreme values. Should I remove them before analysis? Not necessarily. The decision depends on the outlier's cause [53].
- Remove outliers only if they are due to measurement or data entry errors (e.g., an impossible height value of 10.8135 for an adult man) or if they are from a population outside your study's scope (e.g., a subject with diabetes in a study on healthy bone growth) [53].
- Do not remove outliers if they represent a natural variation within the population you are studying. Removing them can make the process appear more predictable than it truly is [53]. Always document any excluded data points and your reasoning [53].
Q2: Which robust measures can I use if I cannot remove outliers? When outliers are a natural part of your data, use statistical methods that are less sensitive to extreme values. The table below compares common robust deviation measures.
| Measure | Calculation | Breakdown Point | Best Use Cases | Efficiency on Normal Data |
|---|---|---|---|---|
| Median Absolute Deviation (MAD) | Median(|Xᵢ - median(X)|) | 50% (Highest) | Maximum robustness required; data with up to 50% outliers [54]. | 37% relative to standard deviation [54]. |
| Interquartile Range (IQR) | Q₃ - Q₁ | 25% | Focusing on central data distribution; creating boxplots; outlier identification [54]. | 50% relative to standard deviation [54]. |
| Trimmed Standard Deviation | Standard deviation after removing a % of extreme values | Depends on trim % | Maintaining familiar interpretation of standard deviation; moderate robustness is sufficient [54]. | 80-95% (depends on trimming) [54]. |
| Qn / Sn Estimator | Based on pairwise differences between data points | Up to 50% | Highest statistical efficiency is needed; small sample sizes; unknown data distribution [54]. | 82-88% relative to standard deviation [54]. |
Q3: What constitutes a 'critical' protocol deviation in a clinical trial? A protocol deviation is considered critical (or important/serious) if it increases potential risk to participants or affects the integrity of study data [55] [56]. This differs from a minor deviation, which is unlikely to have such an impact. Examples of critical deviations include enrolling a patient who does not meet key eligibility criteria or missing a crucial safety assessment [55].
Q4: How do likelihood ratios help in sensitivity analysis? Likelihood ratios (LRs) are valuable because they are not impacted by disease prevalence, unlike predictive values [2]. They quantify how much a diagnostic test result will change the probability of a disease.
- Positive Likelihood Ratio (LR+): How much the probability of disease increases with a positive test result. Formula:
LR+ = Sensitivity / (1 - Specificity)[2]. - Negative Likelihood Ratio (LR-): How much the probability of disease decreases with a negative test result. Formula:
LR- = (1 - Sensitivity) / Specificity[2]. In sensitivity analysis for your models, LRs can help assess the strength of your findings by showing how sensitive your conclusions are to the diagnostic accuracy of the tests or measures used.
Experimental Protocol: Managing Protocol Deviations
Objective: To establish a standardized procedure for identifying, documenting, reporting, and mitigating protocol deviations in a clinical trial setting.
Workflow Overview: The following diagram illustrates the lifecycle of a protocol deviation from discovery to resolution.
Materials & Reagents:
- Protocol Deviation Form (in Rave EDC): A standardized electronic form for capturing deviation details, including discovery date, description, and category [56].
- Corrective and Preventive Action (CAPA) Plan: A formal document outlining steps to address the immediate deviation and prevent its recurrence [56].
- Institutional Review Board (IRB) / Central IRB (CIRB) Reporting Guidelines: The official protocol specifying reporting timelines and requirements for deviations [56].
Procedure:
- Discovery & Identification: Any study staff (site personnel, auditor, central monitor) may discover a deviation. The Site Investigator (or designee) is responsible for its management [56].
- Documentation:
- Reporting:
- Assessment & Review: The Lead Protocol Organization (LPO) reviews the submitted deviation to confirm its classification and determine if it is critical [56].
- Mitigation:
- For critical deviations, define a Mitigation Strategy (CAPA) [56].
- Corrective Action (CA): Address the immediate issue (e.g., re-consent the participant, complete a missed procedure) [56].
- Preventive Action (PA): Implement changes to prevent recurrence (e.g., staff retraining, revision of SOPs) [56].
The Scientist's Toolkit: Research Reagent Solutions
| Tool / Solution | Function | Application Context |
|---|---|---|
| Python with SciPy/NumPy | Provides functions for calculating MAD, IQR, and trimmed standard deviation for robust data analysis [54]. | General data analysis and outlier-resistant inference. |
| Robust Regression (e.g., in R) | Uses bounded influence estimating equations to fit models less distorted by outliers in the outcome variable [57]. | Causal inference and observational studies with contaminated data. |
| Covariate Balancing Propensity Score (CBPS) | A method for estimating propensity scores that explicitly balances covariate distributions between treatment and control groups, enhancing robustness in causal effect estimation [57]. | Observational studies to minimize confounding bias. |
| Protocol Deviation Form (Rave EDC) | Standardized electronic form to ensure consistent reporting and tracking of all protocol departures across clinical trial sites [56]. | Clinical trial management and quality control. |
| Nonparametric Hypothesis Tests | Statistical tests (e.g., Mann-Whitney U) that do not rely on distributional assumptions like normality and are thus robust to outliers [53]. | Analyzing data when outliers cannot be legitimately removed. |
Technical Support Center
Troubleshooting Guides
Guide 1: Diagnosing Overfitting and Underfitting
Problem: Model performance is poor. How do I determine if it's due to overfitting or underfitting?
Diagnostic Flowchart:
Diagnostic Parameters and Interpretations:
| Metric | Underfitting Pattern | Overfitting Pattern | Healthy Pattern |
|---|---|---|---|
| Training Error | High [58] | Very Low [58] [59] | Moderate to Low |
| Test Error | High [58] | Significantly Higher than Training [58] [59] | Similar to Training |
| Bias-Variance | High Bias, Low Variance [59] | Low Bias, High Variance [59] | Balanced |
| Learning Curves | Convergence at high error [58] | Large gap between curves [58] | Convergence with small gap |
Resolution Steps for Underfitting:
- Increase Model Complexity: Switch from linear models to Decision Trees, Random Forests, or Neural Networks [58]
- Enhanced Feature Engineering: Create more informative features from existing data [58]
- Reduce Regularization: Dial back L1/L2 regularization that may be punishing complexity excessively [58]
- Extended Training: Allow more training epochs for complex models [58]
Resolution Steps for Overfitting:
- Gather More Data: Increase training set size with high-quality, relevant data [58]
- Implement Robust Cross-Validation: Use k-fold cross-validation for reliable performance estimation [58] [59]
- Apply Regularization: Use L1/L2 regularization or dropout (for neural networks) to penalize complexity [58] [59]
- Employ Early Stopping: Halt training when validation performance degrades [58] [59]
- Feature Selection: Eliminate redundant or irrelevant features [59]
Guide 2: Implementing Parsimonious Model Selection with Multiple Outcomes
Problem: How do I select a common set of predictors when modeling multiple clinical outcomes simultaneously?
Methodology: Best Average BIC (baBIC) Method [60]
Experimental Protocol:
Normalize BIC for Each Outcome
Where BIC(k) = -2logL + k*log(number of uncensored observations) [60]
Calculate Average Normalized BIC
Compare Against Traditional Methods [60]
Performance Comparison Table:
| Selection Method | Parsimony (Number of Predictors) | Predictive Accuracy (C-statistic) | Use Case |
|---|---|---|---|
| Individual Outcome | Variable per outcome | High for specific outcomes | When outcomes have different predictor sets |
| Union Method | Least parsimonious | High across outcomes | When accuracy is prioritized over simplicity |
| Intersection Method | Most parsimonious | Lowest accuracy | When extreme simplicity is required |
| Full Method (no selection) | No parsimony | Variable, risk of overfitting | When clinical rationale dominates |
| baBIC Method (proposed) | Balanced parsimony | High across outcomes | Optimal balance of accuracy and simplicity |
Frequently Asked Questions
Q1: How can I apply likelihood ratios in diagnostic model development while maintaining parsimony?
A: Likelihood ratios (LRs) help quantify how much a diagnostic test or finding shifts the probability of disease [61]. To maintain parsimony in LR-integrated models:
- Use LRs to identify the most informative predictors: focus on those with LRs farthest from 1 (either positive or negative) as they have the greatest impact on post-test probability [61]
- Calculate LRs as:
- LR+ = sensitivity / (1 - specificity)
- LR- = (1 - sensitivity) / specificity [61]
- Apply Bayesian framework: Post-test odds = Pre-test odds × LR, where odds = P/(1-P) [61]
- Select predictors that provide the greatest change from pre-test to post-test probability while minimizing the total number of predictors
Q2: What practical strategies can I use to find the "Goldilocks Zone" between overfitting and underfitting?
A: Follow this systematic approach: [58]
- Start Simple: Begin with a simple, interpretable model (e.g., Logistic Regression or shallow Decision Tree) to establish a performance baseline
- Diagnose Systematically: Plot learning curves to identify whether your model suffers from high bias (underfitting) or high variance (overfitting)
- Iterate Strategically:
- If underfitting: increase model complexity, add features, reduce regularization
- If overfitting: gather more data, apply regularization, use early stopping
- Validate Rigorously: Final judgment must come from performance on a held-out test set using robust k-fold cross-validation [58]
Q3: How do I implement the baBIC method for multiple outcomes in practice?
A: Implementation workflow: [60]
Q4: What are the most effective regularization techniques for preventing overfitting in complex models?
A: The optimal regularization approach depends on your model type: [58] [59]
| Technique | Best For | Implementation | Parsimony Benefit |
|---|---|---|---|
| L1 Regularization (Lasso) | Linear models, feature selection | Adds absolute value penalty | Automatically selects features by driving coefficients to zero |
| L2 Regularization (Ridge) | Correlated features | Adds squared magnitude penalty | Reduces variance without eliminating features |
| Dropout | Neural networks | Randomly drops neurons during training | Prevents co-adaptation of features |
| Early Stopping | Iterative models | Stops training when validation error increases | Prevents over-optimization on training data |
| Pruning | Decision trees | Removes branches with little predictive power | Simplifies tree structure |
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Parsimonious Model Development:
| Tool/Reagent | Function | Application Context |
|---|---|---|
| k-Fold Cross-Validation | Robust performance estimation | Model evaluation and selection [58] [59] |
| Bayesian Information Criterion (BIC) | Model selection criterion | Balancing goodness-of-fit with complexity [60] |
| Normalized BIC Metric | Cross-outcome comparison | Multiple outcome modeling [60] |
| Likelihood Ratio Calculator | Diagnostic utility assessment | Evaluating predictor importance [61] |
| Learning Curve Generator | Bias-variance diagnostics | Identifying overfitting/underfitting [58] |
| Regularization Parameters | Complexity control | Preventing overfitting [58] [59] |
| Feature Selection Algorithms | Predictor prioritization | Creating parsimonious feature sets [59] |
Experimental Protocol: baBIC Implementation for Clinical Prognostic Models
Background: Developing parsimonious models for multiple clinical outcomes requires specialized methodology beyond single-outcome approaches [60].
Materials and Software Requirements:
- Dataset with multiple time-to-event outcomes
- Statistical software with survival analysis capabilities (R, SAS)
- BIC calculation functions
- Cross-validation utilities
Step-by-Step Methodology:
Define Outcome Set
- Identify M clinical outcomes of interest (e.g., mortality, ADL dependence, mobility decline)
- Ensure adequate event rates for each outcome
Candidate Predictor Specification
- Define full set of potential predictors
- Include clinically relevant variables regardless of statistical significance
Model Fitting and BIC Calculation
Model Selection and Validation
- Select model with minimum baBIC
- Validate using k-fold cross-validation
- Compare performance against Union, Intersection, and Full methods [60]
Expected Outcomes:
- Identification of common predictor subset across multiple outcomes
- Superior balance between parsimony and accuracy compared to traditional methods
- Reduced data collection burden while maintaining predictive performance
Troubleshooting Notes:
- If nBIC values exceed 1, candidate models perform worse than full model—exclude from consideration [60]
- If baBIC differences between models are minimal, consider clinical interpretability as tie-breaker
- Ensure BIC normalization within comparable scales across outcomes [60]
Frequently Asked Questions
Q1: Why should I avoid standard asymptotic methods for very small samples (e.g., n ≤ 5)? Standard asymptotic approximations, like first-order large-sample asymptotics, often perform poorly with very small samples because they are based on the assumption of a large sample size. In small samples, these methods can yield inaccurate critical values and p-values, leading to unreliable inference [62]. Robust methods designed for small samples are necessary to avoid being misled by outliers or model assumptions [63].
Q2: What are robust location estimators, and which should I use for n=3 or n=4? For very small samples, use simple, permutation-invariant, and location-scale equivariant estimators. The median is highly robust. For n=3, the median is recommended as it has a high breakdown point. Avoid the average, which is strongly attracted by outliers [63].
Q3: My model requires a scale estimate. Can I robustly estimate scale for n=3? Robustly estimating scale is challenging for n ≤ 3. For n=2, scale is a multiple of the absolute difference. For n ≥ 4, you can use robust scale estimators like the Median Absolute Deviation (MAD) or the Qn estimator [63].
Q4: What is a good alternative to large-sample asymptotics for test statistics in small samples? Small-disturbance asymptotics can be a more accurate approximation than large-sample asymptotics in many contexts, such as dynamic linear regression models. For example, the small-disturbance asymptotic distribution of a t-test for a dynamic coefficient is Student's t, which is typically more accurate than the standard normal approximation provided by large-sample theory [62].
Q5: How can I perform sensitivity or tipping-point analysis without computationally expensive re-fitting? The Sampling-Importance Resampling (SIR) algorithm allows you to approximate posterior distributions under alternative prior settings without re-running Markov chain Monte Carlo (MCMC) for each one. This is highly efficient for tipping-point analyses where you gradually change a hyperparameter, like the degree of external data borrowing [64].
Troubleshooting Guides
Issue: Outliers are distorting my location estimate in a very small sample
Problem Statement The average (mean) of a very small dataset (n=3 to n=5) is being heavily influenced by a single outlying observation, providing a misleading estimate of the central location [63].
Symptoms or Error Indicators
- The mean value changes dramatically if one data point is removed or altered.
- A large gap exists between the mean and the median of the sample.
- The outlying value is visually distant from the cluster of other points on a dot plot.
Possible Causes
- Measurement inaccuracies or technical problems during data collection.
- Data entry errors.
- The underlying population distribution may have heavy tails.
Step-by-Step Resolution Process
- Visualize the data: Create a simple dot plot or strip chart to identify potential outliers visually.
- Calculate robust summary statistics:
- Compute the sample median.
- Compare it to the mean. A substantial difference indicates the mean is being pulled by outliers.
- For n ≥ 4, consider a robust M-estimator: Use an M-estimator of location with an auxiliary robust scale estimate (like MAD) for increased efficiency, provided the scale can be estimated reliably [63].
- Report the robust estimate: Use the median or M-estimator as your primary location estimate instead of the mean.
Escalation Path or Next Steps If the choice of estimator is critical (e.g., for regulatory submission in drug development), consult a statistician to perform a full sensitivity analysis using methods like SIR to understand the impact of the outlier on final inferences [64].
Validation or Confirmation Step Confirm that the robust estimate (e.g., median) is stable and does not change wildly with the removal of any single data point, unlike the mean.
Issue: Choosing an asymptotic approximation for a test statistic in a dynamic regression model
Problem Statement When testing the coefficient of a lagged-dependent variable in a dynamic linear regression model with a small or moderate sample size, it is unclear whether to use the standard normal or Student's t distribution to obtain critical values or p-values [62].
Symptoms or Error Indicators
- The p-value for the coefficient of the lagged-dependent variable is near the significance threshold.
- Different asymptotic approximations (standard normal vs. Student's t) lead to different conclusions about the statistical significance of the coefficient.
Possible Causes
- The large-sample (standard normal) approximation may be inaccurate in small samples.
- The small-disturbance (Student's t) approximation may be more accurate but is less commonly used.
Step-by-Step Resolution Process
- Identify your test statistic: This guide applies to the t-test statistic for the coefficient α in the model: ( yt = αy{t-1} + zt'β + ut ), with ( u_t ~ IN(0, σ^2) ) [62].
- Compare approximations: Be aware that the large-sample asymptotic distribution is standard normal, while the small-disturbance asymptotic distribution is Student's t [62].
- Prefer the Student's t approximation: Empirical evidence using the Kullback-Leibler Information (KLI) measure suggests the Student's t distribution is typically a more accurate approximation to the true distribution of the test statistic in this context [62].
- Use Student's t critical values: For your significance test, use critical values from the Student's t distribution with degrees of freedom based on your sample size and model.
Validation or Confirmation Step The conclusion about the coefficient's significance should be more reliable and yield better statistical properties (e.g., sizes closer to the nominal level) when using the Student's t approximation [62].
Experimental Protocols & Data Presentation
Table 1: Comparison of Location Estimators for Very Small Samples
| Estimator | Sample Size (n) | Breakdown Point | Key Properties | Recommendation |
|---|---|---|---|---|
| Mean | n ≥ 1 | 0% (Non-robust) | High efficiency under normality, but highly sensitive to outliers. | Avoid in small samples if outliers are suspected [63]. |
| Median | n ≥ 1 | 50% (High) | Highly robust, but less statistically efficient than the mean under normality. | Recommended for n = 3 [63]. |
| M-Estimator | n ≥ 4 | Varies | More efficient than the median; requires a robust auxiliary scale estimate. | Use for n ≥ 4 when an efficient robust estimate is needed [63]. |
Table 2: Comparison of Asymptotic Approximations for the t-test in a Dynamic Regression Model
| Approximation Type | Theoretical Basis | Limiting Distribution | Relative Accuracy (KLI Measure) | Recommendation |
|---|---|---|---|---|
| Large-Sample Asymptotics | Sample size (n) → ∞ | Standard Normal | Less accurate in small samples | Avoid for small samples in dynamic models [62]. |
| Small-Disturbance Asymptotics | Disturbance variance (σ²) → 0 | Student's t | More accurate in small samples | Preferred for small samples in dynamic models [62]. |
Protocol 1: Robust Location and Scale Estimation for n ≤ 5
Purpose: To obtain reliable estimates of a population's central tendency and spread from a very small sample that may contain outliers [63].
Procedure:
- Data Collection: Collect the small sample of measurements (n ≤ 5).
- Location Estimation:
- For n=3: The median is the recommended robust location estimator.
- For n=4 or n=5: The median is a safe choice. For greater statistical efficiency, an M-estimator (e.g., Huber-type) with an auxiliary scale estimate can be used.
- Scale Estimation:
- For n=2: Scale is estimated as a multiple of |x₂ - x₁|.
- For n=3: Reliable robust scale estimation is not generally possible.
- For n ≥ 4: Use the Median Absolute Deviation (MAD) or the Qn estimator.
- Reporting: Report both the robust location and scale estimates, clearly stating the estimators used.
Protocol 2: Efficient Prior Sensitivity and Tipping-Point Analysis via SIR
Purpose: To efficiently evaluate how posterior inferences change under different prior distributions, or to find the "tipping-point" prior hyperparameter where a conclusion changes, without computationally expensive MCMC re-fitting [64].
Procedure:
- Base Model Fitting: Fit your base Bayesian model using MCMC, obtaining M posterior samples for the parameters of interest.
- Define Alternative Priors: Specify the range of alternative prior distributions (e.g., π*(θ; ψ)) you wish to investigate.
- Calculate Importance Weights: For each alternative prior and each posterior sample ( θ{(m)} ) from the base model, compute the importance weight: ( wm \propto π*(θ{(m)}) / π(θ{(m)}) ), and then normalize the weights to sum to 1 [64].
- Check Diagnostic: Calculate the Effective Sample Size (ESS), where ( ESS = 1 / \sum \tilde{w}_m^2 ). A small ESS indicates the reweighting is unreliable.
- Approximate New Posteriors:
- For summaries: Compute the weighted average ( \sum{m=1}^M \tilde{w}m h(θ{(m)}) ) to approximate the posterior expectation under the new prior.
- For samples: Use sampling importance resampling (SIR) to draw a new set of samples from the base samples according to the probabilities ( \tilde{w}m ) [64].
- Find Tipping-Point: To find the hyperparameter ψ where the upper credible interval bound equals a null value θ₀, solve ( Qα(ψ) = θ0 ) using a numerical method like the bisection method, evaluating ( Q_α(ψ) ) at each step using the SIR approach [64].
Workflow Visualizations
Sensitivity Analysis with SIR
Small Sample Analysis Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Analytical Tools for Small Sample Inference
| Tool / Reagent | Function / Purpose | Key Consideration |
|---|---|---|
| Median | A robust estimator of central location for very small samples. | The recommended location estimator for n=3; has a high breakdown point [63]. |
| MAD (Median Absolute Deviation) | A robust estimator of scale. Computed as median(|x_i - median(x)|). | Preferred over the standard deviation for n ≥ 4 when outliers are a concern [63]. |
| Qn Estimator | An alternative robust scale estimator with high efficiency. | A good choice for n ≥ 4; more efficient than MAD [63]. |
| M-Estimators | A class of robust estimators that generalize maximum likelihood estimation. | Useful for n ≥ 4 to gain efficiency; requires a robust auxiliary scale estimate [63]. |
| SIR Algorithm | A computational method for approximating posterior distributions under alternative prior settings without MCMC re-fitting. | Crucial for efficient sensitivity and tipping-point analysis; monitor ESS [64]. |
| Small-Disturbance Asymptotics | An asymptotic theory based on the disturbance variance going to zero. | Provides more accurate approximations (e.g., Student's t) than large-sample theory in some small-sample settings [62]. |
Sensitivity Analysis (SA) is defined as “a method to determine the robustness of an assessment by examining the extent to which results are affected by changes in methods, models, values of unmeasured variables, or assumptions” with the aim of identifying “results that are most dependent on questionable or unsupported assumptions” [8]. In clinical trials, the credibility of results relies heavily on the validity of analytical methods and their underlying assumptions. Sensitivity analyses address crucial "what-if" questions that investigators and readers must consider: Will the results change if different methods of analysis are used? How will protocol deviations or missing data affect the conclusions? What impact will outliers have on the treatment effect? [8]
Pre-specifying sensitivity analyses in the study protocol is critical for maintaining research integrity and reducing bias. When analyses are planned before data collection begins, researchers demonstrate a commitment to transparent and rigorous science, avoiding the perception that analytical choices were made to achieve desired results. The International Council for Harmonisation (ICH) recognizes this importance through guidelines like ICH E9(R1), which introduces the "estimand" framework and emphasizes sensitivity analysis for handling intercurrent events in clinical trials [65].
Frequently Asked Questions (FAQs) on Pre-specifying Sensitivity Analyses
Q1: Why is pre-specification of sensitivity analyses necessary in clinical trial protocols?
Pre-specification of sensitivity analyses in trial protocols is essential for several reasons. First, it demonstrates that researchers have carefully considered potential threats to validity and planned appropriate assessments of robustness before seeing the trial data. Second, it prevents potential bias that could occur if analytical choices were made post-hoc based on which approaches yield the most favorable results. Third, regulatory agencies increasingly expect and sometimes require pre-specified sensitivity analyses. For instance, Health Canada's adoption of ICH E9(R1) emphasizes the importance of defining how intercurrent events will be handled, which typically requires sensitivity analyses to assess robustness [65].
Consistency between primary analysis results and pre-specified sensitivity analyses strengthens confidence in the findings. When sensitivity analyses yield similar conclusions to the primary analysis across various assumptions and methods, the results are considered "robust" [8]. The US Food and Drug Administration (FDA) and European Medicines Agency (EMA) state that "it is important to evaluate the robustness of the results and primary conclusions of the trial" to various limitations of data, assumptions, and analytical approaches [8].
Q2: What types of sensitivity analyses should be pre-specified in a protocol?
Researchers should pre-specify sensitivity analyses that address the key assumptions and potential limitations most relevant to their trial design and context. Common types include:
- Missing Data Handling: Specify alternative approaches for handling missing data beyond the primary method (e.g., multiple imputation, pattern-mixture models) [8].
- Protocol Deviations: Plan analyses that assess the impact of non-compliance, crossovers, or other deviations (e.g., per-protocol analyses) [8].
- Outlier Influence: Pre-specify analyses that examine the effect of extreme values on results [8].
- Model Specification: For model-based analyses, plan variations in model structure or assumptions [66].
- Unmeasured Confounding: In observational components or generalizability assessments, plan analyses like E-values or proxy pattern-mixture models to assess potential unmeasured confounding [66] [67].
The updated SPIRIT 2025 guidelines for trial protocols provide structured guidance on what should be addressed, emphasizing comprehensive pre-specification of analytical methods including sensitivity analyses [68].
Q3: How do I determine the appropriate scenarios for sensitivity analyses?
Selecting appropriate scenarios for sensitivity analyses requires consideration of both clinical and statistical factors. The Representative and Optimal Sensitivity Analysis (ROSA) approach provides a methodological framework for selecting scenarios that effectively represent how a trial's operating characteristics vary across plausible values of unknown parameters [69]. This method uses a utility criterion to identify scenarios that best represent the relationship between unknown parameters and operating characteristics.
When applying this approach:
- Identify the vector of unknown parameters that could influence trial conclusions (e.g., enrollment rates, magnitude of treatment effect, prevalence of biomarkers)
- Define the operating characteristics of interest (e.g., probability of detecting treatment effects, Type I error rate)
- Select scenarios that maximize the utility of representing how operating characteristics vary across the parameter space [69]
For generalizability assessments, the Proxy Pattern-Mixture Model (RCT-PPMM) uses bounded sensitivity parameters to quantify potential bias due to nonignorable selection mechanisms when extending trial results to broader populations [67].
Q4: What are common pitfalls in pre-specifying sensitivity analyses?
Common pitfalls in pre-specifying sensitivity analyses include:
- Vague Specification: Stating that "sensitivity analyses will be conducted" without detailing the specific methods, scenarios, or assumptions to be varied.
- Overly Optimistic Assumptions: Failing to consider clinically realistic scenarios that challenge the primary analysis conclusions.
- Insufficient Justification: Not providing rationale for chosen sensitivity analysis methods or parameters.
- Ignoring Key Limitations: Overlooking important potential sources of bias specific to the trial context.
- Failure to Align with Estimand Framework: Not connecting sensitivity analyses to the handling of intercurrent events as outlined in ICH E9(R1) [65].
Q5: How should results from pre-specified sensitivity analyses be reported?
When reporting pre-specified sensitivity analyses:
- Present results from all pre-specified sensitivity analyses alongside primary results
- Describe any deviations from the pre-specified sensitivity analysis plan
- Discuss the consistency between primary and sensitivity analyses
- Interpret the implications when sensitivity analyses yield meaningfully different results
- Use tables to summarize multiple scenario results for easy comparison [8]
Transparent reporting allows readers to assess the robustness of findings and understand how conclusions might change under different assumptions or methods.
Troubleshooting Common Issues
Problem: Discrepancies Between Primary and Sensitivity Analysis Results
Issue: Pre-specified sensitivity analyses yield meaningfully different results from the primary analysis.
Troubleshooting Guide:
- Assess the magnitude and direction of differences—do they change clinical interpretations?
- Examine whether specific assumptions drive the differences
- Consider additional exploratory analyses to understand sources of discrepancy
- Report all results transparently and discuss possible reasons for discrepancies
- Avoid emphasizing only the most favorable results—maintain scientific integrity
Example: In a cost-effectiveness analysis, Williams et al. found that excluding outliers changed the cost per quality-adjusted life year ratios, indicating that the primary results were sensitive to extreme values [8].
Problem: Handling Unanticipated Data Issues
Issue: Unforeseen data patterns emerge that were not addressed in pre-specified sensitivity analyses.
Troubleshooting Guide:
- Document all unanticipated data issues as they arise
- If possible, conduct additional post-hoc sensitivity analyses to address these issues
- Clearly distinguish between pre-specified and post-hoc analyses in reporting
- Discuss the limitations introduced by unanticipated issues
- For future protocols, consider similar trials' experiences to anticipate potential issues
Problem: Regulatory Concerns About Generalizability
Issue: Regulators question whether trial results apply to broader patient populations.
Troubleshooting Guide:
- Implement generalizability sensitivity analyses like the RCT-PPMM framework [67]
- Use bounded sensitivity parameters to quantify potential selection bias
- Leverage summary-level baseline covariate data from target populations
- Systematically vary sensitivity parameters to determine robustness to departures from ignorable sample selection
- Present a range of plausible treatment effects under different selection scenarios
Methodological Protocols for Sensitivity Analysis
Protocol 1: Sensitivity Analysis for Missing Data
Background: Missing data is inevitable in most clinical trials and can introduce bias if not handled appropriately.
Pre-specification Elements:
- Primary analysis method for handling missing data (e.g., multiple imputation)
- Specific sensitivity analysis approaches (e.g., pattern-mixture models, selection models)
- Assumptions to be varied (e.g., missing at random vs. missing not at random)
- Parameters for different missing data scenarios
Implementation Steps:
- Implement primary analysis method
- Apply pre-specified sensitivity analysis methods under different assumptions
- Compare results across approaches
- Assess whether conclusions are robust to different missing data assumptions
Protocol 2: Sensitivity to Unmeasured Confounding
Background: Unmeasured confounding can bias treatment effect estimates, particularly in non-randomized study components or generalizability assessments.
Pre-specification Elements:
- Primary method for addressing confounding (e.g., propensity score adjustment)
- Sensitivity analysis method (e.g., E-values, proxy pattern-mixture models)
- Range of sensitivity parameters to be explored
- Criteria for assessing robustness
Implementation Steps:
- Conduct primary analysis adjusting for measured confounders
- Calculate E-values to assess the strength of unmeasured confounding needed to explain away results [66]
- For generalizability assessments, implement RCT-PPMM with varying sensitivity parameters [67]
- Determine the range of plausible treatment effects under different confounding scenarios
Protocol 3: Operating Characteristic Evaluation in Complex Designs
Background: Complex trial designs (e.g., adaptive, biomarker-stratified) have operating characteristics that depend on unknown parameters.
Pre-specification Elements:
- Key operating characteristics to evaluate (e.g., power, type I error, probability of correct selection)
- Unknown parameters that influence operating characteristics
- Range of plausible values for unknown parameters
- ROSA method implementation details [69]
Implementation Steps:
- Define utility criterion for scenario selection
- Identify ROSA scenarios that best represent operating characteristic variations
- Compute operating characteristics across selected scenarios
- Evaluate whether design performance is adequate across plausible scenarios
Visualizing Sensitivity Analysis Workflows
Sensitivity Analysis Implementation Workflow
Likelihood Ratio Model Sensitivity Assessment
Research Reagent Solutions for Sensitivity Analysis
Table 1: Essential Methodological Tools for Sensitivity Analysis
| Tool Category | Specific Methods | Primary Function | Implementation Considerations |
|---|---|---|---|
| Missing Data Handling | Multiple Imputation, Pattern-Mixture Models, Selection Models | Assess robustness to missing data assumptions | Pre-specify missing data mechanisms; vary assumptions systematically |
| Causal Inference Sensitivity | E-values, Proxy Pattern-Mixture Models (RCT-PPMM) [67] | Quantify potential unmeasured confounding | Define bounded sensitivity parameters; use summary-level population data |
| Model Specification | Alternative Link Functions, Varying Random Effects Structures | Test robustness of model-based inferences | Pre-specify key model variations; justify clinically plausible alternatives |
| Outlier Influence | Trimming, Winsorizing, Robust Regression Methods | Evaluate impact of extreme values | Define outlier criteria prospectively; compare inclusive and exclusive approaches |
| Generalizability Assessment | Transportability Methods, Selection Bias Adjustments | Extend inferences to target populations | Leverage registry data; specify exchangeability assumptions |
Regulatory and Reporting Considerations
Regulatory agencies globally are increasingly emphasizing sensitivity analysis in clinical trials. The recent adoption of ICH E9(R1) by agencies like Health Canada illustrates the growing importance of the estimand framework and associated sensitivity analyses [65]. The updated SPIRIT 2025 statement provides evidence-based checklist items for trial protocols, including items relevant to sensitivity analysis pre-specification [68].
When pre-specifying sensitivity analyses for regulatory submissions:
- Align with relevant guidelines (ICH E9(R1), FDA/EMA guidance on complex trials)
- Justify choice of sensitivity analysis methods based on trial design and potential biases
- Pre-specify decision criteria for interpreting sensitivity analysis results
- For innovative designs, consider the ROSA approach to demonstrate operating characteristics across plausible scenarios [69]
- For generalizability assessments, incorporate methods like RCT-PPMM when extending results to broader populations [67]
Despite their importance, sensitivity analyses remain underutilized in practice, with only about 26.7% of published papers in major medical journals reporting them [8]. Comprehensive pre-specification in protocols represents a crucial step toward improving this practice and enhancing the credibility of clinical trial results.
Establishing Credibility: Validation Frameworks and Comparative Analysis of Methods
In clinical trials and diagnostic model development, the credibility of results depends heavily on the validity of the methods and assumptions used. Sensitivity analysis (SA) addresses this by determining the robustness of an assessment by examining how results are affected by changes in methods, models, values of unmeasured variables, or assumptions [16]. When evaluating comparative model performance, particularly with likelihood ratio models, SA moves beyond a single best model to explore how conclusions vary under different plausible scenarios.
For researchers and drug development professionals, this approach is fundamental when planning new trials or diagnostic tests. SA helps assess how operating characteristics—such as the probability of detecting treatment effects or expected study duration—vary depending on unknown parameters that exist before a study begins [69]. Regulatory agencies like the FDA and EMA recommend evaluating robustness through sensitivity analyses to ensure appropriate interpretation of results [16].
Core Concepts: Likelihood Ratios and Sensitivity Analysis Frameworks
Understanding Likelihood Ratios in Diagnostic Models
Likelihood ratios (LRs) quantify how much a specific test result will raise or lower the probability of a target disease or condition [70]. They are calculated from the sensitivity and specificity of a diagnostic test and are used to update the probability that a condition exists [61].
- LR+ (Positive Likelihood Ratio): Ratio of the probability of a positive test result in subjects with the condition against the probability of a positive test result in subjects without the condition. Calculated as:
LR+ = sensitivity / (1 - specificity)[61]. - LR- (Negative Likelihood Ratio): Ratio of the probability of a negative test result in subjects with the condition to the probability of a negative test result in subjects without the condition. Calculated as:
LR- = (1 - sensitivity) / specificity[61].
LRs are applied using Bayes' theorem to update disease probability estimates. The pre-test probability (often estimated by clinician judgment or population prevalence) is converted to pre-test odds, multiplied by the appropriate LR, and converted back to post-test probability [61].
Types of Sensitivity Analysis in Clinical Research
Sensitivity analyses assess how changes in key inputs affect model results and conclusions. Common types include [16]:
Table: Types of Sensitivity Analyses in Clinical Research
| Analysis Type | Purpose | Common Applications |
|---|---|---|
| Methods of Analysis | Compare different statistical approaches | Assess robustness to analytical choices |
| Outcome Definitions | Test different cut-offs or definitions | Verify findings aren't definition-dependent |
| Missing Data Handling | Evaluate impact of missing data | Compare complete-case vs. multiple imputation |
| Distributional Assumptions | Test different statistical distributions | Compare parametric vs. non-parametric methods |
| Impact of Outliers | Assess influence of extreme values | Analyze data with and without outliers |
Frequently Asked Questions (FAQs)
Q1: Why is sensitivity analysis particularly important for likelihood ratio models? Sensitivity analysis is crucial for LR models because these models often depend on assumptions that may impact conclusions if unmet. For diagnostic tests using LRs, SA evaluates how changes in sensitivity/specificity estimates, pre-test probability estimates, or missing data handling affect the final diagnostic accuracy and clinical utility [16] [61]. This is especially important since pre-test probability estimates often involve subjective clinician judgment.
Q2: How many sensitivity scenarios should I test when comparing model performance? The number of scenarios represents a trade-off between comprehensiveness and interpretability. While there's no fixed rule, a common challenge is that too many scenarios (e.g., 100+) make results difficult to interpret and communicate [69]. The Representative and Optimal Sensitivity Analysis (ROSA) approach provides a methodological framework for selecting an optimal set of scenarios that adequately represents how operating characteristics vary across plausible parameter values [69].
Q3: What constitutes "robust" findings in sensitivity analysis? Findings are considered robust when, after performing sensitivity analyses under different assumptions or methods, the conclusions remain consistent with those from the primary analysis [16]. If modifying key assumptions doesn't substantially change the treatment effect or model performance conclusions, researchers can be more confident in their findings.
Q4: How should I handle missing data in sensitivity analyses for comparative trials? A recommended approach is to:
- Conduct primary analysis under the Missing at Random (MAR) assumption using methods like multiple imputation
- Perform sensitivity analyses exploring Not Missing at Random (NMAR) scenarios using methods like Delta-Adjusted multiple imputation or pattern mixture models
- Compare results under different missing data mechanisms to assess robustness [17]
Q5: Are likelihood ratios validated for use in series with multiple diagnostic tests? No. While some clinicians use one LR to generate a post-test probability and then use this as a pre-test probability for a different test's LR, this sequential application has not been validated in research. LRs have never been validated for use in series or in parallel, and there's no established evidence to support or refute this practice [61].
Troubleshooting Guides
Handling Non-Robust Results in Sensitivity Analysis
Problem: Sensitivity analyses reveal that conclusions change substantially when altering methods, assumptions, or handling of outliers.
Solution Protocol:
- Quantify the Impact: Determine which specific modifications cause conclusions to change. For example, note if results become non-significant when using multiple imputation instead of complete-case analysis for missing data [16].
- Report Transparently: Clearly document both primary and sensitivity analysis results, noting where conclusions are fragile [16].
- Contextualize Findings: Discuss possible reasons for non-robustness in the study context. For example, if outlier exclusion changes conclusions, describe potential reasons for these extreme values [16].
- Consider Design Modifications: For future studies, consider adjustments to minimize identified vulnerabilities, such as improved data collection methods to reduce missing data [17].
Addressing Computational Challenges in Simulation-Based SA
Problem: Running comprehensive sensitivity analyses with multiple parameters and scenarios is computationally intensive.
Solution Protocol:
- Implement the ROSA Framework: Use the Representative and Optimal Sensitivity Analysis method to select a parsimonious set of scenarios that maximizes representation of how operating characteristics vary across parameters [69].
- Leverage Efficient Design: Use optimization techniques like simulated annealing and flexible regression methods like neural networks to approximate operating characteristics without exhaustive simulation [69].
- Prioritize Parameters: Focus on parameters with greatest uncertainty and potential impact on conclusions, rather than performing exhaustive variations of all parameters [69].
Diagram: Computational Workflow for Efficient Sensitivity Analysis
Managing Diagnostic Test Uncertainty in Likelihood Ratio Models
Problem: Uncertainty in sensitivity and specificity estimates leads to wide confidence intervals in likelihood ratios, reducing diagnostic utility.
Solution Protocol:
- Quantity Uncertainty: Calculate confidence intervals for sensitivity and specificity, then propagate this uncertainty to LRs [61].
- Pre-specify Analyses: Determine important sensitivity scenarios in advance, such as best-case, worst-case, and most-plausible values for sensitivity/specificity [16].
- Contextualize with Pre-test Probability: Remember that test utility depends on how much LRs can change probability from pre-test to post-test levels. Even tests with moderate LRs can be useful when pre-test probability is intermediate [61].
- Consider Spectrum Bias: Assess whether sensitivity/specificity estimates came from populations similar to your target population, as spectrum bias can affect LR performance [61].
Experimental Protocols for Key Analyses
Protocol for Sensitivity Analysis of Missing Data in Time-to-Event Studies
Purpose: To assess robustness of time-to-event analysis conclusions to different assumptions about missing time-dependent covariates [17].
Materials and Reagents: Table: Research Reagent Solutions for Missing Data Analysis
| Item | Function | Example Implementation |
|---|---|---|
| Multiple Imputation by Chained Equations (MICE) | Creates multiple complete datasets by imputing missing values | mice package in R |
| Delta-Adjusted Multiple Imputation | Incorporates sensitivity parameters for NMAR data | Custom modification of imputation algorithm |
| Cox Proportional Hazards Model | Analyzes time-to-event data with covariates | coxph function in R |
| Martingale Residual Calculation | Assesses model fit and informs imputation | Residuals from Cox model |
Methodology:
- Specify Missing Data Mechanism: Define whether missingness is assumed MCAR, MAR, or NMAR based on study design and missing data patterns [17].
- Implement Primary Analysis:
- Use Multiple Imputation under MAR assumption
- Incorporate event-time information in imputation model using martingale residuals or including event indicator, event/censoring time, and logarithm of time [17]
- Conduct Sensitivity Analyses:
- Apply Delta-Adjusted MI with varying δ values to represent different magnitudes of departure from MAR
- Use pattern mixture models with different identifying assumptions
- Compare results across approaches [17]
- Interpret Findings: Compare treatment effect estimates and significance conclusions across different missing data handling methods.
Diagram: Sensitivity Analysis Workflow for Missing Data
Protocol for Simulation-Based Sensitivity Analysis of Trial Designs
Purpose: To evaluate and compare operating characteristics of candidate clinical trial designs across plausible scenarios of unknown parameters [69].
Methodology:
- Define Parameter Space: Identify vector of unknown parameters (e.g., enrollment rates, treatment effects, biomarker prevalence) and their plausible ranges [69].
- Select Operating Characteristics: Determine relevant performance metrics (e.g., probability of detecting treatment effects, type I error rate, expected sample size) [69].
- Implement ROSA Framework:
- Use flexible regression methods (e.g., neural networks) to approximate relationship between parameters and operating characteristics
- Apply optimization algorithm (e.g., simulated annealing) to select optimal set of scenarios that best represent variations in operating characteristics across parameter space [69]
- Run Simulations: For each selected scenario, compute operating characteristics using trial simulations or analytic results.
- Generate Sensitivity Report: Present scenarios and corresponding operating characteristics in structured tables, highlighting how characteristics vary across parameter space [69].
Advanced Applications and Integration
Integrating Sensitivity Analysis with Likelihood Ratio Reporting
When reporting likelihood ratios from diagnostic models, comprehensive sensitivity analysis should address:
- Spectrum Effects: Assess how LRs vary across patient subgroups or disease severity spectra [61]
- Threshold Effects: Evaluate how different test positive thresholds affect LR values and clinical utility [16]
- Verbal vs. Numerical Presentations: Explore comprehension differences when presenting LRs numerically versus with verbal strength-of-support statements [7]
Recent research indicates that existing literature doesn't definitively answer what presentation method maximizes understandability of LRs for legal decision-makers, highlighting the need for careful sensitivity analysis in communication formats [7].
Bayesian Approaches to Sensitivity Analysis
Bayesian methods offer natural frameworks for sensitivity analysis through:
- Prior Distributions: Assessing how conclusions change with different prior specifications [16]
- Posterior Predictive Checks: Comparing observed data to replicated data from the model
- Probabilistic Sensitivity Analysis: Propagating uncertainty from all parameters simultaneously
These approaches are particularly valuable for likelihood ratio models, where Bayesian updating naturally incorporates pre-test probabilities and test results to generate post-test probabilities [61].
FAQs on Cross-Validation and External Validation
1. What is the fundamental difference between internal and external validation?
- Internal validation assesses the expected performance of a model on data drawn from a population similar to the original training sample. Techniques like cross-validation and bootstrapping are used, where the test data is randomly selected from the same dataset used for training [71] [72].
- External validation evaluates how well a model performs on data collected from a completely independent source, such as a different hospital, geographic location, or patient population. This tests the model's generalizability to new, unseen settings [71] [73] [72].
2. When should I use k-fold cross-validation instead of a simple holdout method?
K-fold cross-validation is particularly advantageous when working with small to moderately sized datasets, which are common in healthcare and clinical research [74] [75]. In k-fold cross-validation, the data is split into k subsets (or folds). The model is trained k times, each time using k-1 folds for training and the remaining one fold for testing, and the results are averaged [76] [77]. This method provides a more reliable estimate of model performance than a single holdout split because it uses all data for both training and testing, reducing the high variance and uncertainty that can plague a single, small holdout set [71].
3. Our model performed well in internal cross-validation but poorly on a new dataset. What are the likely causes?
This is a classic sign of overfitting and a lack of generalizability. Common causes include [71]:
- Population Differences: The new dataset may come from a patient population with different characteristics (e.g., disease stage, demographics, co-morbidities) than the development cohort.
- Over-optimism in Internal Validation: Internal validation can still produce optimistic performance estimates if the data is not perfectly representative or if the model is too complex.
- Data Quality or Procedural Differences: Variations in data collection methods, measurement techniques, or equipment between the development and new settings can degrade performance.
4. How does nested cross-validation improve the model selection process?
Nested cross-validation provides a less biased way to perform both model selection (e.g., choosing hyperparameters) and performance evaluation simultaneously [74] [75]. It involves two layers of cross-validation:
- An inner loop is used to tune the model's hyperparameters.
- An outer loop is used to evaluate the model's performance after it has been tuned in the inner loop. This strict separation prevents information about the test set from "leaking" into the model training and tuning process, leading to a more realistic estimate of how the model will perform on external data [74].
Troubleshooting Guides
Issue 1: High Variance in Cross-Validation Performance Estimates
Problem: When running k-fold cross-validation, the performance metric (e.g., AUC) varies significantly from one fold to another.
Solutions:
- Increase the Number of Folds: Try using 10-fold instead of 5-fold cross-validation. Using more folds means each training set is larger and more similar to the overall dataset, which can stabilize the estimate [74] [75].
- Use Repeated Cross-Validation: Perform k-fold cross-validation multiple times (e.g., 5 times 10-fold) with different random data splits and average the results. This helps smooth out variability caused by a particularly "easy" or "hard" test fold [77].
- Stratify Your Folds: For classification problems, especially with imbalanced outcomes, use stratified k-fold cross-validation. This ensures that each fold has approximately the same proportion of class labels as the complete dataset, preventing folds with no positive cases [74] [75].
Issue 2: Model Fails During External Validation
Problem: A model that showed excellent discrimination and calibration during internal validation performs poorly on an external dataset.
Solutions:
- Analyze Population Drift: Before applying the model, compare the distributions of key predictor variables and outcomes between your development and external validation cohorts. Significant differences may indicate the model needs to be recalibrated or updated for the new population [71] [73].
- Consider Model Updating: Rather than discarding the model, you can update it for the new setting. Techniques include:
- Recalibration: Adjusting the intercept or slope of the model to align predictions with observed outcomes in the new population.
- Model Revision: Re-estimating a subset of the model's coefficients using data from the new population.
- Use Subject-Wise Splitting from the Start: If your data has multiple records per patient (e.g., repeated hospital visits), ensure your internal validation uses subject-wise splitting. This means all records from a single patient are kept together in either the training or test set. Using record-wise splitting can lead to over-optimistic performance by allowing the model to "learn" patient-specific patterns that won't generalize to new individuals [74] [75].
Issue 3: Choosing Between AIC and BIC for Model Selection in Sensitivity Analysis
Problem: When using likelihood ratio models for sensitivity analysis, Akaike's Information Criterion (AIC) and the Bayesian Information Criterion (BIC) support different models, creating ambiguity.
Solutions:
- Understand Their Emphasis: View AIC and BIC through the lens of sensitivity and specificity. AIC is designed for good prediction and is more sensitive to complex models, which can lead to a higher risk of overfitting (false positives). BIC emphasizes parsimony and is more conservative, with a higher risk of underfitting (false negatives) [78].
- Align Criterion with Research Goal:
- If your goal is predictive accuracy, such as developing a prognostic tool, AIC may be preferable.
- If your goal is identifying the "true" underlying model with a strong theoretical foundation, BIC is often the better choice [78].
- Report Both: In the context of sensitivity analysis for a thesis, it can be informative to report results from both criteria to demonstrate the robustness (or sensitivity) of your findings to different model selection philosophies [78].
Experimental Protocols & Data
Protocol 1: Implementing k-Fold Cross-Validation
This protocol outlines the steps for performing k-fold cross-validation to estimate model performance [76].
- Data Preparation: Clean and preprocess the entire dataset (e.g., handle missing values).
- Define Folds: Randomly partition the dataset into k equally sized subsets (folds). For classification, use stratified sampling to preserve class distribution in each fold.
- Iterative Training and Validation: For each of the k iterations:
- Training Set: Use k-1 folds to train the model.
- Test Set: Use the remaining 1 fold to test the model.
- Score: Calculate the desired performance metric (e.g., AUC, accuracy) on the test set.
- Performance Estimation: Compute the mean and standard deviation of the k performance scores from the previous step. The mean is the cross-validated estimate of model performance.
Protocol 2: Conducting an External Validation Study
This protocol describes the process for a rigorous external validation of a pre-existing model [73].
- Model Acquisition: Obtain the full specification of the model to be validated, including all predictor variables, their coefficients, and the required data pre-processing steps.
- Cohort Definition: Define an independent validation cohort from a different source (e.g., a different hospital, time period, or geographical region). Apply the same inclusion and exclusion criteria as the original development study, if possible.
- Data Collection and Adjudication: Collect the necessary predictor and outcome data for the new cohort. For objective outcomes like drug-induced thrombocytopenia, a multidisciplinary panel should independently review and adjudicate cases based on pre-defined criteria (e.g., temporal relationship to drug exposure, platelet count recovery) [73].
- Model Application: Apply the pre-existing model to the new cohort's data without re-estimating any parameters.
- Performance Assessment: Evaluate model performance on the external cohort using measures of discrimination (e.g., Area Under the ROC Curve - AUC), calibration (e.g., calibration slope and plot), and clinical utility (e.g., decision curve analysis).
Table 1: Comparison of Internal Validation Methods on a Simulated Dataset (n=500) This table summarizes a simulation study comparing internal validation techniques, showing the performance and uncertainty associated with each method [71].
| Validation Method | AUC (Mean ± SD) | Calibration Slope | Key Characteristics |
|---|---|---|---|
| 5-Fold Cross-Validation | 0.71 ± 0.06 | Comparable | Lower uncertainty than holdout; uses all data efficiently. |
| Holdout (80/20 Split) | 0.70 ± 0.07 | Comparable | Higher uncertainty due to single, small test set. |
| Bootstrapping | 0.67 ± 0.02 | Comparable | Provides stable performance estimates. |
Table 2: Impact of External Test Set Size on Performance Estimation Based on simulation results, this table shows how the size of the external test set affects the precision of the performance estimate [71].
| External Test Set Size | Impact on AUC Estimate | Impact on Calibration Slope SD |
|---|---|---|
| n = 100 | Less precise estimate | Larger standard deviation |
| n = 200 | More precise estimate | Smaller standard deviation |
| n = 500 | Most precise estimate | Smallest standard deviation |
Table 3: Model Selection Criteria Comparison This table compares the properties of common information criteria used for model selection in likelihood-based models [78].
| Criterion | Penalty Weight | Emphasis | Likely Kind of Error |
|---|---|---|---|
| AIC | ( 2k ) | Good prediction | Overfitting (False Positive) |
| BIC | ( k \cdot \log(n) ) | Parsimony | Underfitting (False Negative) |
Workflow Diagrams
Cross-Validation vs External Validation
k-Fold Cross-Validation Workflow
The Scientist's Toolkit
Table 4: Essential Reagents and Computational Tools for Validation Experiments
| Item / Tool | Function / Purpose |
|---|---|
| Stratified k-Fold Cross-Validator | A function (e.g., StratifiedKFold in scikit-learn) that splits data into folds while preserving the percentage of samples for each class, crucial for imbalanced datasets [76] [74]. |
| Nested Cross-Validation Pipeline | A computational framework that implements an inner loop for hyperparameter tuning and an outer loop for performance estimation, preventing optimistic bias [74] [75]. |
| Calibration Plot | A diagnostic plot to assess the agreement between predicted probabilities and observed outcomes. A slope < 1 indicates overfitting and the need for recalibration, especially after external validation [71] [73]. |
| SHAP (SHapley Additive exPlanations) | A method from cooperative game theory used to interpret the output of any machine learning model. It helps identify key predictor variables and understand their contribution to model predictions, which is vital for explaining model behavior in new populations [73]. |
| Information Criteria (AIC/BIC) | Model selection tools based on penalized likelihood. They provide a standardized way to balance model fit and complexity, helping to choose between candidate models during development and sensitivity analysis [78]. |
Frequently Asked Questions (FAQs)
R-squared
Q1: My linear regression model has a high R-squared value, but my colleague says it might still be a poor fit. Is this possible?
Yes, this is possible and highlights a key limitation of relying solely on R-squared. A high R-squared indicates the percentage of variance in the dependent variable explained by your model, but it does not guarantee the model is unbiased or adequate [79] [80]. You can have a high R-squared value while your model suffers from specification bias, such as missing important predictor variables, polynomial terms, or interaction terms [79]. This often manifests as a pattern in the residual plots, where the model systematically over- and under-predicts the observed values [80]. Always complement R-squared analysis with residual plots and other goodness-of-fit statistics [79].
Q2: In my field, R-squared values are consistently low. Does this mean our models are not useful?
Not necessarily. In fields that attempt to predict complex outcomes like human behavior, low R-squared values are common and expected [79] [80]. A low R-squared value indicates a high degree of unexplainable variance in your data, which is inherent to some disciplines [79]. The most important consideration is the statistical significance of your predictor variables. If your independent variables are statistically significant, you can still draw important conclusions about the relationships between variables, even with a low R-squared [79] [80].
ROC Curves
Q3: When I compare two nested logistic regression models using ROC curves, the AUC test is not significant, but the Wald test for the new marker is. Which result should I trust?
You should trust the Wald test (or likelihood ratio test) from the underlying regression model. Research has demonstrated that using the standard Area Under the Curve (AUC) test to compare fitted values from nested regression models (e.g., a model with and without a new predictor) produces invalid results [81]. The test statistic and its estimated variance can be seriously biased in this context, leading to exceptionally conservative test size and low power. Therefore, the Wald or likelihood ratio tests remain the preferred approach for testing the incremental contribution of a new marker in a regression model [81].
Q4: The ROC curve for my diagnostic test has an Area Under the Curve (AUC) of less than 0.5. What does this mean, and how can I fix it?
An AUC less than 0.5 suggests that your diagnostic test performs worse than random chance [82]. This typically occurs due to an incorrect "test direction" [82]. When setting up the ROC analysis, you must specify whether a larger or smaller test result indicates a more positive test (i.e., a higher likelihood of the condition of interest). If this direction is set incorrectly, the ROC curve will descend toward the lower right, and the AUC will be below 0.5 [82]. To remedy this, re-run your analysis and correctly specify the test direction in the software options [82].
Q5: Two ROC curves from different models intersect. Can I still use the AUC to decide which model is better?
Simply comparing the total AUC values is insufficient when ROC curves intersect [82]. The AUC summarizes performance across all possible thresholds, but if one curve is superior in a specific region (e.g., high-sensitivity range) and the other is superior in a different region (e.g., high-specificity range), the total AUC can be misleading [82]. In this case, you should use the partial AUC (pAUC), which computes the area over a clinically relevant range of false positive rates (FPR) or true positive rates (TPR) [82]. Additionally, consider other metrics like accuracy, precision, and recall to provide a comprehensive assessment tailored to your diagnostic scenario [82].
Goodness-of-Fit Tests
Q6: Beyond R-squared, what are some robust statistical methods for assessing the goodness-of-fit of a model?
Two common statistical methods for assessing goodness-of-fit are the F-test and Equivalence Testing.
- F-Test: This test compares the lack-of-fit error to the pure (random) error in your data. It determines if the lack-of-fit is significant compared to the inherent noise. A significant p-value (e.g., < 0.05) indicates a poor fit. A key limitation is that it requires true replicates at each dose level and can unfairly fail very precise assays due to small pure error [83].
- Equivalence Testing: This is often the regulator-preferred method. Instead of testing for a significant difference, it tests whether a model is "close enough" to a better one. For example, to test a 4-parameter logistic (4PL) model, you might fit a 5PL model and check if the confidence interval for its additional parameter falls entirely within pre-defined equivalence limits around the 4PL value. This method avoids the precision penalty but requires historical data to set meaningful equivalence limits [83].
Troubleshooting Guides
Issue 1: Interpreting a High R-squared Value
Problem: A regression model shows a high R-squared value, but predictions are inaccurate.
| Step | Action | Principle & Rationale |
|---|---|---|
| 1 | Plot Residuals vs. Fitted Values | A well-fitting model has residuals that are randomly scattered around zero. Any systematic pattern (e.g., a curve) indicates bias [79] [80]. |
| 2 | Check for Omitted Variable Bias | The model may be missing important predictors, polynomial terms, or interaction terms, leading to systematic under/over-prediction [79]. |
| 3 | Consider Nonlinear Regression | If the data follows a curve, a linear model will be biased regardless of R-squared. A nonlinear model may be more appropriate [80]. |
| 4 | Validate with Out-of-Sample Data | Check if the high R-squared results from overfitting the sample's random quirks. Use cross-validation or a holdout sample to assess performance on new data [79]. |
Issue 2: Determining the Optimal Cut-off Point for a Diagnostic Test
Problem: You need to determine the best threshold to classify subjects as positive or negative for a condition using a continuous biomarker.
Diagram: Workflow for Optimal Cut-point Determination
The following table summarizes common methods for selecting the optimal cut-point [84].
| Method | Formula / Principle | Clinical Use Case |
|---|---|---|
| Youden Index | J = max[ Sensitivity + Specificity - 1 ] | Balances sensitivity and specificity equally. A general-purpose method when both error types are equally important [84]. |
| Euclidean Index | D = min[ √(1-Sensitivity)² + (1-Specificity)² ] | Identifies the point on the ROC curve closest to the perfect test point (0,1). Often yields results similar to the Youden Index [84]. |
| Product Index | P = max[ Sensitivity * Specificity ] | Maximizes the product of sensitivity and specificity. Can produce results similar to the Youden and Euclidean methods [84]. |
| Diagnostic Odds Ratio (DOR) | DOR = (LR⁺)/(LR⁻) | Not recommended for cut-point selection as it often produces extreme, non-informative values and is inconsistent with other methods [84]. |
Note: Always consider the clinical context. For a screening test, you may prioritize high sensitivity, while for a confirmatory test, high specificity might be more critical.
Issue 3: Comparing the Diagnostic Accuracy of Two Tests
Problem: You need to statistically compare the Area Under the Curve (AUC) of two ROC curves derived from the same subjects.
| Step | Action | Principle & Rationale |
|---|---|---|
| 1 | Determine the Study Design | Are the tests applied to the same subjects (paired design) or different subjects (independent design)? This determines the correct statistical test [82] [85]. |
| 2 | Select the Appropriate Test | For a paired design, use the DeLong test [82] [85]. For independent samples, use a method like Dorfman and Alf [82]. Using the wrong test invalidates results. |
| 3 | Check for Curve Intersection | If the ROC curves cross, a comparison of total AUC can be misleading. Use partial AUC (pAUC) to focus on a clinically relevant range of specificities or sensitivities [82]. |
| 4 | Report Supplementary Metrics | Alongside the AUC test, report metrics like accuracy, precision, and recall to give a comprehensive view of performance [82]. |
Research Reagent Solutions
This table details key analytical "reagents" (statistical tests and tools) essential for quantitative assessment in sensitivity analysis and diagnostic model evaluation.
| Tool / Test | Function | Key Considerations |
|---|---|---|
| R-squared (R²) | Measures the proportion of variance in the dependent variable explained by a linear model [79] [80]. | Does not indicate model bias. Always use with residual plots. Low values can be acceptable in some fields [79] [80]. |
| Adjusted R-squared | Adjusts R-squared for the number of predictors in the model, penalizing unnecessary complexity [79]. | More reliable than R-squared for comparing models with different numbers of predictors [79]. |
| Residual Plots | Visual tool to detect non-random patterns, bias, and violations of model assumptions [79] [83]. | Fundamental for diagnosing a poorly specified model, regardless of R-squared [79] [80]. |
| F-Test for Lack-of-Fit | Compares lack-of-fit error to pure error to assess model adequacy [83]. | Requires true replicates. Can unfairly penalize highly precise data. Less suitable with pseudoreplicates [83]. |
| DeLong Test | Compares correlated ROC curves (from the same subjects) based on the AUC [82] [85]. | The standard nonparametric test for paired designs. Preferred over methods that assume binormality [85]. |
| Equivalence Testing | Tests if a model is statistically "equivalent" to a more complex one, rather than just "not different" [83]. | Preferred by regulators for model selection (e.g., 4PL vs. 5PL). Requires historical data to set equivalence limits [83]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between a Pattern-Mixture Model (PMM) and a Selection Model (SM)?
The fundamental difference lies in how they factorize the joint distribution of the outcome variable (Y) and the missing data mechanism (R). PMMs factorize this joint distribution as the marginal distribution of the missingness pattern multiplied by the conditional distribution of the outcome given the missingness pattern (f(Y|R) * f(R)). In contrast, SMs factorize it as the marginal distribution of the outcome multiplied by the conditional distribution of missingness given the outcome (f(Y) * f(R|Y)) [86] [87]. Practically, this means PMMs group individuals based on their pattern of missing data (e.g., drop-out time) and model the outcomes within each group, while SMs model the probability of data being missing as a function of the (potentially unobserved) outcome values [88] [86].
Q2: When should I choose a Pattern-Mixture Model over a Selection Model for my sensitivity analysis?
Choose a Pattern-Mixture Model when your goal is to make the assumptions about the unobserved data explicit and transparent [88]. PMMs are often considered more intuitive for clinicians and applied researchers because they directly postulate what the missing data might look like in different dropout patterns [88] [89]. They are particularly useful when you want to specify a range of plausible scenarios for the missing data, often controlled via sensitivity parameters, and then assess how the results change (δ in the diagram below) [87] [88] [89].
Q3: My data has a multilevel structure (e.g., patients within clinics). How can I implement these models? For multilevel data, such as in Cluster Randomized Trials (CRTs), the model must account for the hierarchical structure. When using PMMs, one effective approach is to combine them with multilevel multiple imputation [88]. This involves:
- Grouping individuals with the same dropout time into patterns.
- Using multilevel imputation models that include random effects for clusters to impute missing values under a Missing at Random (MAR) assumption.
- Then, modifying these imputed values using pre-specified sensitivity parameters (
k) to create Missing Not at Random (MNAR) scenarios for a sensitivity analysis [88]. This method ensures that the within-cluster correlation is properly accounted for, preventing falsely narrow confidence intervals.
Q4: What are the key "sensitivity parameters," and how do I choose values for them? Sensitivity parameters are quantities that cannot be estimated from the observed data and are used to encode specific MNAR assumptions [87] [88].
- In Pattern-Mixture Models: The sensitivity parameters are often differences in the outcome between observed and unobserved individuals within the same dropout pattern [88] [89]. For example, you might assume that individuals who dropped out have a worse outcome by a certain amount (
k). - In Selection Models: The sensitivity parameters are typically the coefficients that link the unobserved outcome to the probability of that outcome being missing [86]. Choosing values is a matter of clinical or scientific judgment. A recommended practice is to perform a tipping point analysis, where you vary the sensitivity parameter over a plausible range of values and observe at what point the primary conclusion of the study changes (e.g., from significant to non-significant) [88] [89].
Q5: Can I implement these models in a Bayesian framework? Yes, a Bayesian framework is highly suitable for both PMMs and SMs [87] [86]. The Bayesian approach naturally incorporates uncertainty about the sensitivity parameters through their prior distributions. You can specify informative prior distributions for the sensitivity parameters based on expert opinion or previous studies. The analysis then yields posterior inferences that directly reflect the influence of these pre-specified assumptions [87]. Furthermore, Bayesian software that implements Gibbs sampling can often be used to fit these models [87].
Troubleshooting Guides
Issue 1: My Pattern-Mixture Model is "Under-Identified"
Problem: You receive an error or the model fails to converge because the PMM is under-identified. This means that within some missingness patterns (e.g., among dropouts), there is no information to estimate the parameters for the unobserved outcomes [88].
Solution: Apply identifying restrictions or use the Pattern-Mixture Model with Multiple Imputation (PM-MI) approach [88] [89].
- Step 1: Fit a model to the observed data, accounting for the missingness patterns.
- Step 2: Use multiple imputation to create
mcomplete datasets under an MAR assumption. - Step 3: Introduce a sensitivity parameter (
korδ) to shift or scale the imputed values for specific dropout patterns, creating MNAR conditions. - Step 4: Analyze each of the
mMNAR-adjusted datasets and pool the results using Rubin's rules [88] [89]. This process overcomes under-identification by making explicit assumptions about the missing data.
Issue 2: Interpreting Results from Multiple Sensitivity Analyses
Problem: You have run multiple models (PMMs and SMs) with different sensitivity parameters and now have a range of results. You are unsure how to draw a final conclusion.
Solution: Follow this decision workflow:
Interpreting the Workflow:
- Primary Analysis: Begin with your primary analysis, typically under the MAR assumption [88].
- Assess Robustness: If the substantive conclusion (e.g., "Treatment A is superior to Treatment B") remains unchanged across all plausible MNAR scenarios explored with PMMs and SMs, your results are considered robust [89].
- Handle Sensitivity: If the conclusion changes, you must report this sensitivity. Identify the "tipping point"—the specific assumption at which the conclusion changes—and report the full range of possible treatment effects [88] [89].
Issue 3: Selecting Covariates for the Imputation or Data Model
Problem: You are unsure which variables to include in your imputation model (for PMM) or your data model (for SM).
Solution: Including the correct variables is critical for a valid analysis, especially under MAR.
- What to Include: Your model should include all variables that are part of the substantive analysis model, as well as any other variables that are predictive of the outcome or predictive of missingness [90]. In longitudinal studies, this includes baseline outcomes and time-varying covariates that may be associated with the outcome or dropout [87] [89].
- What to Avoid: A naive complete-case analysis or a model that omits key predictors of missingness, as this can lead to biased estimates, even under MAR [90].
Key Methodologies and Experimental Protocols
Protocol 1: Implementing a Basic Pattern-Mixture Model with Multiple Imputation
This protocol provides a step-by-step guide for implementing a PMM using the multiple imputation framework for a longitudinal clinical trial [88] [89].
Research Reagent Solutions
| Item/Technique | Function in the Analysis |
|---|---|
Multiple Imputation Software (e.g., R packages mice) |
Creates multiple "complete" datasets by replacing missing values with plausible ones. |
Sensitivity Parameter (k or δ) |
A user-defined value that quantifies the departure from the MAR assumption. |
| Multilevel Imputation Model | An imputation model that includes random effects for clusters (e.g., clinic ID) to maintain the data structure in CRTs. |
Statistical Analysis Software (e.g., R, SAS, Stata) |
Used to analyze each of the completed datasets and to pool the results. |
Methodology:
- Define Dropout Patterns: Group individuals based on the time at which they dropped out of the study (e.g., Pattern 1: Completed study; Pattern 2: Dropped out at month 3) [88].
- Impute under MAR: Use multiple imputation, with the necessary multilevel structure, to create
mdatasets (e.g.,m=20) where missing values are imputed based on the observed data. This assumes MAR within each pattern. - Apply Sensitivity Parameter: For each imputed dataset, modify the imputed values in the dropout patterns. A common approach is a delta-adjustment:
Y_imp_MNAR = Y_imp_MAR + δ, whereδis the sensitivity parameter [88] [89]. The value ofδcan be different for each treatment arm and dropout pattern. - Analyze and Pool: Perform the primary analysis (e.g., a mixed-effects model) on each of the
mMNAR-adjusted datasets. Pool the parameter estimates (e.g., the treatment effect) and their standard errors using Rubin's combination rules [88] [90]. - Repeat for Sensitivity Analysis: Repeat steps 2-4 for a range of plausible
δvalues to create a sensitivity analysis.
Protocol 2: Specifying a Selection Model for Dropout
This protocol outlines the process for building a Selection Model to handle informative dropout.
Methodology:
- Specify the Measurement Model: Define a model for the longitudinal outcome. This is often a mixed-effects model:
y_ijk = β_0 + β_1(Time_ijk) + β_2(Trt_i) + β_3(Trt_i × Time_ijk) + γ_i + ν_ij + ε_ijkwhereγ_iandν_ijare cluster and individual random effects, respectively [88]. - Specify the Dropout Model: Define a model for the probability of dropout (or being missing). This is typically a logistic or probit regression model that depends on the outcome. For example:
logit(P(R_ij = 1)) = α_0 + α_1 * y_ij[86] Here,R_ij=1indicates the data is observed, and the model states that the probability of observing the data depends on the value of the outcomey_ij(which may be missing). - Joint Estimation: Estimate the parameters of both the measurement and dropout models simultaneously, often using maximum likelihood or Bayesian methods. The coefficient
α_1in the dropout model acts as a sensitivity parameter. If it is statistically different from zero, it provides evidence for an MNAR mechanism [86].
Model Comparison and Selection Table
The following table provides a structured comparison of Pattern-Mixture and Selection Models to guide researchers in selecting the appropriate paradigm.
| Aspect | Pattern-Mixture Model (PMM) | Selection Model (SM) |
|---|---|---|
| Core Factorization | f(Outcome | Missingness) * f(Missingness) [86] |
f(Outcome) * f(Missingness | Outcome) [86] |
| Intuitive Appeal | High; directly models what happens to dropouts [88] | Lower; models the risk of dropping out [88] |
| Handling Under-Identification | Requires explicit constraints (e.g., δ-adjustment) [88] |
Model is identified but can be unstable [88] |
| Primary Use Case | Sensitivity Analysis by creating specific "what-if" scenarios [89] | Direct hypothesis testing about the missing data mechanism [86] |
| Implementation | Often via Multiple Imputation with post-imputation adjustments [88] [89] | Often via joint maximum likelihood or Bayesian estimation [87] [86] |
| Sensitivity Parameters | Differences in outcomes between observed/missing groups (δ) [88] |
Coefficients linking the outcome to missingness probability (α) [86] |
Conceptual Diagram of Model Factorizations
The diagram below illustrates the core difference in how Pattern-Mixture and Selection Models conceptualize the relationship between the outcome data and the missingness mechanism.
I have gathered information on creating accessible flowcharts and diagrams, which are essential for transparent research reporting. However, the available search results do not contain specific troubleshooting guides, experimental protocols, or quantitative data related to sensitivity analysis likelihood ratio models.
Here is a technical support guide synthesized from the available information on designing accessible scientific diagrams.
Troubleshooting Guide: Diagram and Flowchart Accessibility
Q1: My flowchart is complex. How can I make it accessible to colleagues using assistive technologies?
A: For complex flowcharts, a visual diagram alone is insufficient. Provide a text-based alternative that conveys the same logical structure and relationships [91].
- Problem: A complex visual diagram cannot be fully understood through a simple image description.
- Solution:
- Create a Text Version: Use nested lists or headings to represent the chart's hierarchy and decision paths. For a decision flowchart, this sounds like: "If X, then go to Y." For an organizational chart, use heading levels to represent reporting structure [91].
- Provide a Accessible Visual:
- Export the entire flowchart as a single, high-quality image (e.g., via screenshot) to prevent assistive technology from reading each shape as a separate, confusing element [91].
- Write succinct alt-text for the image that summarizes its purpose and directs the reader to the detailed text version, for example: "Flowchart of the model selection process. Detailed text description is provided in Appendix A." [91].
Q2: I need to use color to convey information in my diagram. How can I ensure it is accessible to everyone?
A: Color should not be the only means of conveying information.
- Problem: Readers with color vision deficiencies may miss information relayed only by color [92].
- Solution:
- Use Multiple Cues: Combine color with different shapes, labels, line styles (dashed, dotted), or texture patterns [91].
- Check Contrast: Ensure sufficient contrast between text and its background, and between graphical elements (like arrows and symbols) and their background. The Web Content Accessibility Guidelines (WCAG) require a minimum contrast ratio of 3:1 for large text and graphical objects [93] [92].
- Use a Coherent Palette: Limit your palette to 4-5 colors from the same family to maintain a professional feel and avoid visual confusion [94] [95].
Q3: The automatic layout from my diagramming tool is unclear. How can I improve it?
A: Automated layouts can sometimes produce overlapping lines or illogical flows.
- Problem: The automated layout is messy, making the flowchart difficult to follow.
- Solution:
- Simplify: If the chart is too large, break it into multiple, simpler, linked diagrams [91] [94].
- Follow Conventions: Design the flow to follow a natural reading direction, typically from left to right or top to bottom [94].
- Ensure Clear Paths: Use clean, non-intertwining lines. Readers should easily trace the path from one element to the next without solving a puzzle [94].
The Scientist's Toolkit: Research Reagent Solutions for Clear Diagrams
This table details key "reagents" or essential elements for creating effective and accessible research diagrams.
| Item/Reagent | Function & Explanation |
|---|---|
| Consistent Design Elements | Uses unified shapes, lines, and spacing to simplify perception and allow viewers to process information faster [94]. |
| High-Contrast Color Pairs | Ensures text and graphical elements stand out against the background, which is critical for readability and meeting accessibility standards [93] [92]. |
| Text-Based Equivalents | Provides a textual version (lists, headings) of the visual diagram, ensuring the information is accessible to users of assistive technology and is reproducible [91]. |
| Semantic Shapes | Employs conventional shapes (e.g., rectangle for process, diamond for decision) to provide immediate visual cues about the type of step or data [96]. |
| Alt-Text (Alternative Text) | A brief description of a non-text element (like an image) that is read aloud by screen readers, making the content accessible to visually impaired users [91]. |
Diagram Specifications and Workflow
For all diagrams, adhere to the following specifications to ensure accessibility and clarity:
- Max Width:
760px - Color Contrast Rule: Use the provided color palette. Always check that the contrast ratio between foreground (text, arrows) and background meets WCAG guidelines. A contrast checker tool can be used for verification [93].
- Node Text Contrast: The
fontcolormust be explicitly set to have high contrast against the node'sfillcolor. - Color Palette:
#4285F4,#EA4335,#FBBC05,#34A853,#FFFFFF,#F1F3F4,#202124,#5F6368
Experimental Workflow for Transparent Reporting
The following diagram, generated from the DOT script below, outlines a general workflow for ensuring transparency and reproducibility in research reporting, incorporating accessibility best practices for all produced figures.
Conclusion
Sensitivity analysis is not merely a supplementary step but a fundamental component of rigorous statistical inference with likelihood ratio models. This synthesis demonstrates that proactively testing the robustness of findings against assumptions about unmeasured confounding, missing data, and model specification is crucial for drawing credible conclusions in biomedical research. The methodologies discussed—from simple parameter variations to advanced delta-adjusted multiple imputation—provide a powerful toolkit for quantifying uncertainty. For future directions, the integration of these techniques into standard practice for drug safety monitoring and observational comparative effectiveness research will be paramount. As models grow in complexity, the development of accessible computational tools and standardized reporting guidelines for sensitivity analyses will further enhance the reliability and translational impact of research for drug development professionals and clinical scientists, ultimately leading to more confident decision-making in healthcare.
References
- 1. Likelihood Ratios [https://www.cebm.ox.ac.uk/resources/ebm-tools/likelihood-ratios]
- 2. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 3. Text has minimum contrast[proposed] | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/afw4f7/proposed/]
- 4. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 5. Material Design Color Chart [https://htmlcolorcodes.com/color-chart/material-design-color-chart/]
- 6. Color - Style [https://m1.material.io/style/color.html]
- 7. What is the best way to present likelihood ratios? A review ... [https://www.sciencedirect.com/science/article/pii/S1355030625001261]
- 8. A tutorial on sensitivity analyses in clinical trials: the what, why ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-13-92]
- 9. Evaluating the agreement between sensitivity and primary ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04199-4]
- 10. Performance of location-scale models in meta-analysis [https://pubmed.ncbi.nlm.nih.gov/40097863/]
- 11. Sensitivity Analysis for Causal Inference | Online Course [https://statisticalhorizons.com/seminars/sensitivity-analysis-causal-inference/]
- 12. Application of empirical likelihood ratio test in AR(1) time ... [https://www.nature.com/articles/s41598-025-24076-7]
- 13. Sensitivity Analysis Methods to Know for Causal Inference [https://fiveable.me/lists/sensitivity-analysis-methods]
- 14. Efficiency and Robustness of Causal Effect Estimators ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6647029/]
- 15. A Practical Guide to Sensitivity Analysis for Causal Effects ... [https://bookdown.org/glorya_hu/MNAR-Guide/]
- 16. A tutorial on sensitivity analyses in clinical trials: the what, why ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3720188/]
- 17. Sensitivity analysis for time-to-event data accounting ... [https://www.nature.com/articles/s41598-025-09599-3]
- 18. Examining the Effect of Missing Data and Unmeasured ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11554740/]
- 19. How to Avoid Sensitivity Analysis Pitfalls in Stata [https://www.linkedin.com/advice/0/what-some-common-pitfalls-challenges-sensitivity]
- 20. Developing robust workflows for data science and analytics [https://myadlm.org/cln/articles/2025/julyaugust/developing-robust-workflows-for-data-science-and-analytics]
- 21. Introduction To Robust Design (Taguchi Method) [https://www.isixsigma.com/robust-design-taguchi-method/introduction-robust-design-taguchi-method/]
- 22. Robust parameter design [https://en.wikipedia.org/wiki/Robust_parameter_design]
- 23. Drug Development Tools: Fit-for-Purpose Initiative [https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tools-fit-purpose-initiative]
- 24. Research Tools and Resources [https://www.fda.gov/drugs/science-and-research-drugs/research-tools-and-resources]
- 25. Likelihood Ratio Test - Evolution and ... [https://evomics.org/resources/likelihood-ratio-test/]
- 26. Likelihood-ratio test [https://en.wikipedia.org/wiki/Likelihood-ratio_test]
- 27. The Likelihood Ratio Test [https://towardsdatascience.com/the-likelihood-ratio-test-463455b34de9/]
- 28. 8.4.5 Likelihood Ratio Tests [https://www.probabilitycourse.com/chapter8/8_4_5_likelihood_ratio_tests.php]
- 29. Flexible quantitative bias analysis for unmeasured in... confounding [https://pubmed.ncbi.nlm.nih.gov/40348970/]
- 30. Flexible quantitative bias analysis for unmeasured in... confounding [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02551-z]
- 31. (PDF) Addressing in comparative... unmeasured confounding [https://www.academia.edu/128462234/Addressing_unmeasured_confounding_in_comparative_observational_research]
- 32. Likelihood-Ratio-Test Methods for Drug Safety Signal ... [https://pubmed.ncbi.nlm.nih.gov/30915153/]
- 33. Likelihood-Ratio-Test Methods for Drug Safety Signal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6399568/]
- 34. Likelihood ratio test-based method for signal detection in ... [https://pubmed.ncbi.nlm.nih.gov/23331230/]
- 35. Bayesian hierarchical model for safety signal detection in ... [https://www.sciencedirect.com/science/article/abs/pii/S1551714420302615]
- 36. [2101.07934] Meta-analysis of Censored Adverse Events [https://arxiv.org/abs/2101.07934]
- 37. Sources of Safety Data and Statistical Strategies for Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5987777/]
- 38. Sensitivity analysis for time-to-event data accounting ... [https://pubmed.ncbi.nlm.nih.gov/40707517/]
- 39. Sensitivity Analyses for Missing in Repeatedly Measured ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503996/]
- 40. Tipping Point Sensitivity Analysis for Missing Data in Time ... [https://arxiv.org/abs/2506.19988]
- 41. 3. Sensitivity Analysis: The Basics [https://uc-ebook.org/docs/html/3_sensitivity_analysis_the_basics.html]
- 42. Practical methods for incorporating summary time-to-event ... [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-025-02752-z]
- 43. Evaluating the agreement between sensitivity and primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220123/]
- 44. Sensitivity Analysis - NCBI - NIH [https://www.ncbi.nlm.nih.gov/sites/books/NBK126178/]
- 45. A new likelihood model for analyses of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8265059/]
- 46. Presenting Author(s) - 2025 ISPE Annual Meeting [https://2025ispe.eventscribe.net/ajaxcalls/PresentationInfo.asp?efp=Tk1LT0NQWksyNTAwMQ&PresentationID=1646127&rnd=0.4528282]
- 47. Guidelines for Good Pharmacoepidemiology Practices (GPP) [https://www.pharmacoepi.org/resources/policies/guidelines-08027/]
- 48. 3.4 Model misspecification - Intro To Econometrics [https://fiveable.me/introduction-econometrics/unit-3/model-misspecification/study-guide/D4ujia0pKYhgzOE4]
- 49. Variance Reduction Techniques [https://www.geeksforgeeks.org/data-science/variance-reduction-techniques/]
- 50. What is an intuitive way to think about why high variance in ... [https://stats.stackexchange.com/questions/583754/what-is-an-intuitive-way-to-think-about-why-high-variance-in-predictions-is-asso]
- 51. Bias–variance tradeoff [https://en.wikipedia.org/wiki/Bias%E2%80%93variance_tradeoff]
- 52. Simplifying Common Method Variance Mitigation: The Role ... [https://link.springer.com/article/10.1007/s10869-025-10074-z]
- 53. Guidelines for Removing and Handling Outliers in Data [https://statisticsbyjim.com/basics/remove-outliers/]
- 54. Robust Deviation Measures: Handling Outliers in Data ... [https://medium.com/@shivakumarg814/robust-deviation-measures-handling-outliers-in-data-analysis-13c1871f9757]
- 55. Managing Protocol Deviations: A Guide for Clinical Trials [https://intuitionlabs.ai/articles/managing-protocol-deviations]
- 56. Protocol Deviation User Guide [https://www.ctsu.org/master/simplepage.aspx?ckey=ProtocolDeviations-Guide]
- 57. Doubly robust outlier-resistant inference on causal ... [https://arxiv.org/html/2507.17439v2]
- 58. Overfitting and Underfitting 2025 Avoid the Biggest Mistakes [https://w3schools.cloud/avoid-the-biggest-overfitting-and-underfitting/]
- 59. What is Overfitting? | IBM [https://www.ibm.com/think/topics/overfitting]
- 60. A Novel Method for Identifying a Parsimonious and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8098121/]
- 61. Diagnostics and Likelihood Ratios, Explained [https://thennt.com/diagnostics-and-likelihood-ratios-explained/]
- 62. A comparison of the accuracy of asymptotic approximations ... [https://www.sciencedirect.com/science/article/abs/pii/S0264999314004611]
- 63. Robust estimation in very small samples [https://www.sciencedirect.com/science/article/abs/pii/S0167947302000786]
- 64. Efficient Prior Sensitivity and Tipping-point Analysis for ... [https://arxiv.org/html/2510.10034v1]
- 65. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 66. Sensitivity Analysis (Chapter 12) [https://www.cambridge.org/core/books/multivariable-analysis/sensitivity-analysis/2B59EC7C4DF1706FBAB622AA2A4FBE59]
- 67. A Sensitivity Analysis Framework Using the Proxy Pattern ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593313/]
- 68. SPIRIT 2025 Statement Updated Guideline for Protocols of ... [https://www.ovid.com/journals/jama/pdf/10.1001/jama.2025.4486~spirit-2025-statement-updated-guideline-for-protocols-of]
- 69. Sensitivity Analyses of Clinical Trial Designs [https://pmc.ncbi.nlm.nih.gov/articles/PMC11052542/]
- 70. Likelihood ratios - Measures of diagnostic accuracy [https://analyse-it.com/docs/user-guide/diagnostic-performance/likelihood-ratio]
- 71. External validation: a simulation study to compare cross ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9464671/]
- 72. What is the difference between external and internal cross ... [https://stats.stackexchange.com/questions/492367/what-is-the-difference-between-external-and-internal-cross-validation]
- 73. Development and external validation of a machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261740/]
- 74. Practical Considerations and Applied Examples of Cross ... [https://ai.jmir.org/2023/1/e49023]
- 75. Practical Considerations and Applied Examples of Cross ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11041453/]
- 76. 3.1. Cross-validation: evaluating estimator performance [https://scikit-learn.org/stable/modules/cross_validation.html]
- 77. Cross-validation (statistics) [https://en.wikipedia.org/wiki/Cross-validation_(statistics)]
- 78. Sensitivity and specificity of information criteria - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7299313/]
- 79. How To Interpret R-squared in Regression Analysis [https://statisticsbyjim.com/regression/interpret-r-squared-regression/]
- 80. Regression Analysis: How Do I Interpret R-squared and ... [https://blog.minitab.com/en/blog/adventures-in-statistics-2/regression-analysis-how-do-i-interpret-r-squared-and-assess-the-goodness-of-fit]
- 81. Comparing ROC Curves Derived From Regression Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC3617074/]
- 82. Four overlooked errors in ROC analysis: how to prevent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171508/]
- 83. R² II: What should you use to measure Goodness-of-Fit? [https://www.quantics.co.uk/blog/r%C2%B2-ii-what-should-you-use-to-measure-goodness-of-fit/]
- 84. Methods of determining optimal cut-point of diagnostic ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02198-2]
- 85. Comparing correlated ROC curves for continuous ... [https://www.sciencedirect.com/science/article/abs/pii/S016794730800354X]
- 86. Bayesian pattern-mixture models for dropout and ... [https://link.springer.com/article/10.3758/s13428-023-02128-y]
- 87. Bayesian sensitivity of incomplete data: bridging... analysis [https://pubmed.ncbi.nlm.nih.gov/25256610/]
- 88. A pattern-mixture model approach for handling missing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5628153/]
- 89. An application of a pattern-mixture model with multiple ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-018-0639-y]
- 90. Variable Selection in the Presence of Missing Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC5659333/]
- 91. Key Considerations for Flowchart Accessibility - MN.gov [https://mn.gov/mnit/about-mnit/accessibility/news/?id=38-436349]
- 92. Understanding Success Criterion 1.4.3: Contrast (Minimum) [https://www.w3.org/WAI/WCAG21/Understanding/contrast-minimum.html]
- 93. Contrast Checker [https://webaim.org/resources/contrastchecker/]
- 94. How to Design an Outstanding Flowchart? [https://www.flowmapp.com/blog/qa/how-to-design-flowcharts]
- 95. Choosing Color to Improve your Diagrams [https://creately.com/blog/diagrams/choosing-color-to-improve-your-diagrams/]
- 96. Mermaid FlowChart Basic Syntax [https://docs.mermaidchart.com/mermaid-oss/syntax/flowchart.html]